As FDG-PET enters the mainstream of clinical oncology, it is proving to be particularly adept in the nuts and bolts of staging and disease management. In newly diagnosed non-small cell lung cancer (NSCLC), Australian researchers found that PET provides "powerful prognostic stratification" that is highly appropriate to therapeutic needs. In another study, PET was just as effective following potentially curative therapy.
Writing in the November Journal of Nuclear Medicine, Drs. Rodney Hicks, Victor Kalff, and colleagues from the Peter MacCallum Cancer Center in East Melbourne, Australia discussed their experience with 153 patients who were newly diagnosed with NSCLC (November 2001, 42:11; pp. 1596-1604).
"Surgery remains the mainstay of attempts to cure [NSCLC], but postsurgical prognosis remains poor," they wrote. "Radical radiotherapy, particularly if combined with platinum-based chemotherapy, can be curative in patients with unresectable disease."
But planning either surgery or radical radiotherapy requires both accurate staging of locoregional disease and the exclusion of metastatic disease in appropriate patients, they wrote.
Certainly, CT can't do the job alone. Contrast-enhanced CT, the standard noninvasive modality used in conventional staging, has poor positive and negative predictive values in mediastinal disease in most published series. But PET has been shown to be far more accurate than CT in comparative studies. Moreover, invasive techniques such as mediastinoscopy are not appropriate for most NSCLC patients, less than a third of whom are eligible for surgery, the authors wrote.
The team studied 153 consecutive patients for whom either surgery or radiotherapy was being considered, in an effort to discern "the ability of PET to affect patient management, and more important, to provide prognostic stratification determined by survival."
Staging and disease management pre- and post-PET were compared to results of staging using CT and clinical information. The patients, 102 men and 51 women (mean age 66 ± 9 years), all had newly diagnosed NSCLC. Patients with mixed tumors containing both NSCLC and small cell lung cancer were excluded, as were those with unresectable systemic metastases as confirmed by anatomic imaging. Seventy-four patients had squamous cell carcinomas, 54 had adenocarcinoma, 21 patients had large cell carcinomas, and 4 had unspecified NSCLC, the authors wrote.
A Penn-PET 300-H scanner (UGM Medical Systems, Philadelphia) was used to acquire emission data from the lower neck, thorax, and upper abdomen in all patients; anatomic coverage was extended in all patients to include any areas deemed suspicious in conventional imaging. The researchers processed the emission data using iterative reconstruction both with and without attenuation correction. An experienced nuclear medicine physician reviewed both sets of images with knowledge of previous imaging and clinical information; however, standardized uptake values (SUV) were not routinely calculated, according to the article.
Staging routinely relied on spiral contrast-enhanced CT imaging results, as well as bone scans in all but asymptomatic patients with stage IA disease. Staging was performed in accordance with the 1997 update of the international staging system for lung cancer (Chest, 1997;111 pp:1711-1717).
Patients were assigned a pre-PET tumor, node, metastasis (TNM) stage based on all available information. Mediastinal and hilar lymph nodes larger than 1 cm in diameter were considered positive.
To assess PET's impact on management, clinicians were asked what the management plan would be if PET were not available; post-PET treatment was determined from the medical record or by direct contact with the physician, the authors wrote.
The Kaplan-Meier product-limit method was used to estimate survival, and the results compared using the Cox proportional hazards progression model. Hazard ratios representing the death rate for a given group were compared to a baseline group to determine the prognostic significance of individual factors.
Survival was measured from the date of the PET scan to the date of death from any cause. Median follow-up from the date of the PET scan to the closeout date was 17 months.
"To assess the prognostic value of incorporating the PET findings into the staging process, we compared estimated survival for the pre-PET stage with that for the post-PET stage," the authors wrote. "We also compared survival based on whether curative or palliative treatment was planned before and after PET."
According to the results, the post-PET stage was different from the conventionally determined stage in 65% of the patients. For broad groupings of stage, PET imaging downstaged 10% of cases and upstaged 33%, while 58% of patients remained at the same stage. The original stage did not affect the probability of a change in stage (p=0.35), nor did the presence of equivocal findings in conventional imaging affect the likelihood of stage migration.
 |
Eleven percent of patients with stage I or II disease in anatomical imaging were upgraded to stage IV disease with PET, and 24% were upgraded to stage III. Overall, PET had a high impact on 35% of patients. Therapy was changed from curative to palliative in 22% of patients, and from palliative to curative in 4% of patients. PET changed the modality of treatment but not the therapeutic intent in 9% of patients.
Moreover, post-PET staging was significantly more accurate than pre-PET staging for predicting survival. Each increase in the pre-PET stage was associated with a 29% increase in the death rate, while each increase in post-PET staging was associated with a 69% average increase in the death rate.
Based on these results, the authors concluded that staging that incorporated PET provided a more accurate prognostic stratification than staging with conventional imaging alone, and that PET appropriately changed the management in most patients.
"Overall, PET altered management in 61% of patients," they wrote. "Our findings extend the evidence that PET findings affect clinical decision-making in surgical candidates to a broader spectrum of lung cancer patients typical of a tertiary oncology facility providing radiation oncology services." The information is important because less than a third of patients with newly diagnosed NSCLC are suitable for surgery, they added.
"By allowing patients with a poor prognosis to be converted from futile curative therapy, PET spares them unwarranted morbidity, and spares the community the costs associated with such treatment," they concluded.
PET also superior following treatment
The Australian researchers presented a second study in the same issue, using similar methods to assess whether FDG-PET is useful and predictive of outcome in patients who have undergone potentially curative therapy (Journal of Nuclear Medicine, November 2001, Vol. 42:11; pp. 1605-1613).
In 63 NSCLC patients with suspected relapse more than six months following therapy (mean: 19 months), they compared restaging with conventional imaging and pathological results to those methods with the addition of PET imaging. The Cox proportional hazards regression model was used to evaluate the prognostic significance.
PET findings were positive in 41 of 42 patients with confirmed relapse, with sensitivity of 98%, specificity of 82%, and overall accuracy of 93%. Over 12 months, no disease was found in 14 of 15 patients with clinically suspected relapse but who received a negative PET scan, resulting in a negative predictive value of 93%.
PET results altered disease management significantly in 40 patients, including 6 who were changed from curative to palliative care after PET showed more extensive disease than had been shown on conventional evaluation. Moreover, 8 patients were spared active palliative therapy that was being considered until PET results showed no recurrence of disease.
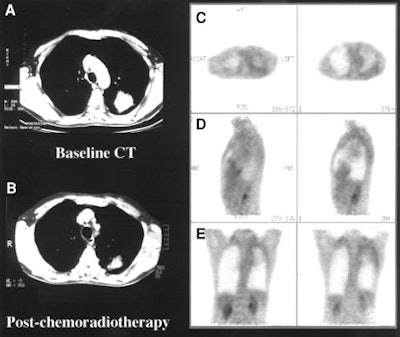 |
The authors found that PET is superior to conventional staging alone in assessing disease status, stratifying prognosis, and selecting patients for treatment, and thus affects patient management significantly.
"Our study suggests that PET, in addition to accurately confirming or excluding disease relapse, more accurately assesses the distribution of disease than do conventional techniques," the authors wrote. "This accuracy is particularly important in patients for whom the PET result altered management."
PET should be performed on patients with suspected relapse following treatment, they concluded, particularly when active treatment is being considered.
By Eric BarnesAuntMinnie.com staff writer
November 5, 2001
Related Reading
Postoperative radiotherapy warranted in some non-small-cell lung cancer patients, September 28, 2001
PET Imaging in Bronchogenic Carcinoma, August 29, 2001
Meta-analysis finds FDG PET far superior to CT in lung cancer staging, November 1, 1999
Copyright © 2001 AuntMinnie.com