Molecular imaging specialists may have unraveled part of the mystery as to why some locally advanced breast cancers (LABC) are impervious to initial chemotherapy -- a discovery that could help oncologists change treatment plans in the short term and develop much better treatments down the road.
Researchers at the University of Washington in Seattle have uncovered a striking consistency among LABC: Those tumors that will ultimately resist chemotherapy can be identified just two months into treatment by their persistent and preserved blood flow.
This connection between vascularity and chemotherapy resistance is described in a newly published study by collaborators in UW’s nuclear medicine, medical oncology, and pathology divisions (Journal of Nuclear Medicine, November 2003, Vol. 44:11, pp. 1806-1814).
An on-site cyclotron enabled the UW radiologists to check tumor blood flow with 15O- water PET scans -- an option not available to most oncologic centers because of 15O’s two-minute half-life. But the link established by the researchers may nonetheless be of interest to all facilities using FDG-PET to predict tumor response to chemotherapy.
"This provides additional insights into how to interpret the results that you get from the application of FDG-PET to this setting," said lead author Dr. David Mankoff, Ph.D., an associate professor of radiology at UW.
Rather than offering a replacement for current FDG-PET tumor studies, "we’re just trying to help understand what we see," Mankoff said in an interview with AuntMinnie.com. "My hunch is that what we’re seeing is a manifestation of tumor biology, rather than blood flow being important per se in the resistance."
The current standard of care for LABC -- generally defined as tumors larger than 5 cm in diameter -- calls for neoadjuvant chemotherapy because such tumors would not be resectable at that size. In more than 70% of LABC cases, that chemotherapy succeeds in shrinking the tumor by 50% or more.
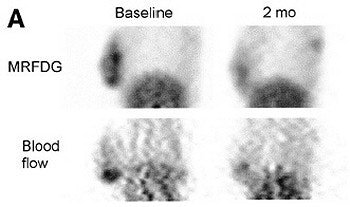 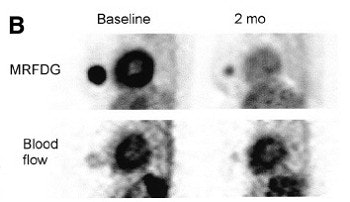 |
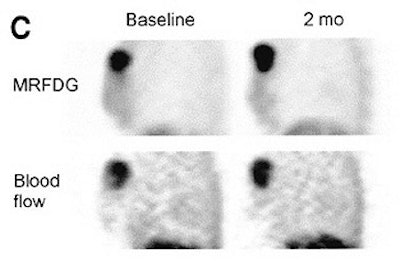
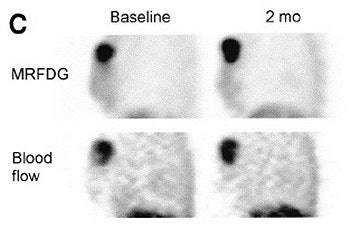
Thick sagittal images of breast and chest patients before therapy (above) and after two months of therapy (below) showing 18F-FDG and 15O-water uptake. 18F-FDG images are summed images of data 30-60 minutes after injection; 15O-water images are summed 30-60 seconds after injection. Patient with macroscopic complete response (A), patient with partial response (PR), and patients with no response (C) are shown. Reprinted by permission of the Society of Nuclear Medicine from: Mankoff, D., et al. Changes in Blood Flow and Metabolism in Locally Advanced Breast Cancer Treated with Neoadjuvant Chemotherapy. J Nucl Med 2003, 44:1806-1814.
 |
But for those cases where chemotherapy isn’t going to help, oncologists need to know as soon as possible so they can alter their treatment plan. That’s where PET can be of assistance.
"If you knew that the tumor wasn’t responding," said Mankoff, "there are enough different forms of chemotherapy and systemic therapy in breast cancer that you could try a different version and see if it works. With breast cancer in this day and age, if therapy A doesn’t work, it doesn’t mean you’re doomed to failure."
Nonetheless, time is of the essence because the prognosis for chemo-resistant LABC is relatively poor. "We did pick two months (as the interval for follow-up after initiation of chemotherapy) with the idea of the earliest possible assessment," Mankoff said, noting that other studies have found some predictive power with FDG-PET after the first cycle of chemotherapy.
Mankoff and his multidisciplinary collaborators are continuing to use their unusual imaging to analyze the promise of new therapies in current clinical trials. "We can do a relatively small number of patients and get a very sophisticated and detailed assessment of how the therapy is working, and perhaps get some insights into why it is or isn’t working," he said.
And in the longer term, he hopes the UW findings can be translated back to a laboratory setting to aid research into even newer treatments for chemo-resistant tumors that can then be brought back to the clinical setting. "Imaging," Mankoff noted, "is one of those pieces that allows you to move back and forth quickly."
By Tracie L. ThompsonAuntMinnie.com staff writer
November 28, 2003
Related Reading
Molecular imaging advocate promotes innovative breast cancer research, October 30, 2003
FDG shows promise as therapeutic agent for metastatic breast cancer, August 27, 2003
PET outperforms CT in breast cancer staging, May 7, 2003
Pinhole technique abets dedicated breast SPECT imaging, April 24, 2003
Positron emission mammography shows promise for breast imaging, October 28, 2002
Copyright © 2003 AuntMinnie.com