Dedicated breast CT scanners aren't on the market yet, or even close to market, truth be told. But breast CT happens every day -- with every chest and cardiac CT exam -- and it's the radiologist's job to read the scan for the frequent incidental findings it can yield. CT can even be used to guide breast intervention in some cases.
"Every chest CT is a breast CT," said Dr. Jeffrey Mendel, in a talk at the 2007 International Symposium on Multidetector-Row CT sponsored by Stanford University. Mendel is chief of radiology at Caritas St. Elizabeth's Medical Center in Boston. He reminded his audience to look at the edges of CT scans to pick up lesions that might otherwise be missed.
Multidetector-row CT (MDCT) actually does a good job of detecting breast lesions, Mendel said. It allows for very thin (1-mm thick) images of the breast so that even small, radiographically visible lesions can be detected on CT.
On the other hand, "only 85% of the breast tissue is visualized on the standard screening mammogram, and ... with breast implants in place that may drop 75% or even 70%," Mendel said. "Many patients coming to you for a CT scan may be ill enough that they haven't had their routine screening mammogram. My mentor ... taught me that we're responsible for the corners of the film, and ... to look at the periphery of the chest and look for the breast tissue."
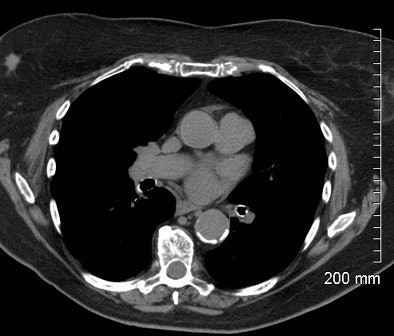 |
| Incidental breast cancer was detected at chest CT in a 65-year-old woman presenting for workup of an incidental nodule on chest x-ray. The patient's last screening mammogram was 18 months before CT. Image courtesy of Dr. Jeffrey Mendel. |
When examining breast tissue, Mendel said radiologists should look for the following:
- Masses or areas of focal asymmetry
- Focal skin thickening
- Architectural distortion
- Radiating spicules reaching to a mass
There's no urgent need to look for microcalcifications, since most are too small to pick up on the average CT scan, Mendel said. But incidental breast carcinomas are found frequently. Mendel said his facility detected four during a typical three-month period last year.
CT intervention
Along with examination of breast data, there are good reasons to perform CT-guided breast intervention, Mendel said. First, if the facility performs breast MRI, it may encounter technical problems that prevent the completion of some MR-guided biopsies.
Among the challenges of MR-guided breast biopsy is that lesions near the chest wall or medially located are very difficult to biopsy with a grid-based technique, he said. The patient has to lie prone for long periods of time, and it's very difficult to monitor and sedate patients in the MR environment.
Also, some incidental breast lesions seen on CT are not visible using MRI or ultrasound.
"In a lot of tertiary care centers, the people who do mammography don't do CT, and they're not really familiar with the capabilities of our MDCT scanners," Mendel said. "So if you think about it, you may find (CT) a nice adjunct to your practice."
Two interventional procedures that are easily performed with a CT scanner are:
- Core needle biopsy -- for patients who can't be safely imaged with MRI, or simply can't tolerate the longer scan times associated with MR-guided breast biopsy
- CT-guided needle localization for surgical incision -- a good choice for lesions that can only be seen on MRI or CT
Certain locations, such as the chest wall, posterior breast, and subareolar, or superficial lesions that cannot be accessed with MR are better performed with CT, Mendel said.
A typical patient presented with an enhancing lesion in the axillary tail -- so far back it was inaccessible to the biopsy grid, Mendel said. She was given contrast to enhance the lesion, turned on her back, and with CT and a thin needle for guidance the lesion was easily excised and a hematoma aspirated, in about 20 minutes with iodinated core biopsy.
During biopsy it's important to place a small metallic marker to allow for future needle localization, he said. Many MR-detected lesions are small and may be completely excised during the biopsy procedure.
Also, do a postprocedural CT scan to ensure that the marker is actually where the lesion was, Mendel advised. This should be followed by a postprocedural mammogram to see if the marker is visible on mammography, and to make sure the marker hasn't moved. The CT scanner is also a great tool for some body biopsies, he said.
CT's advantages include supine positioning and easy patient positioning, Mendel said. With CT, "you can lift the arm up or down, draw blood, you can get access to lesions, you can sedate and monitor your patients easily, and the ultrasound machine doesn't get dragged into the bore of the magnet if you try to put the patient through a CT scanner," he noted.
A challenge of CT is that the breast moves a bit. And although the technique is very straightforward, it is uncommon and so requires a little planning.
The slice thickness depends on lesion size; Mendel said his facility typically uses 3-mm-thick slabs. The dose can be cut fourfold by reducing the kVp to 90 without reducing mAs, he said. Contrast is not always necessary -- for example, when looking for parenchymal asymmetry seen on mammography.
If contrast is administered, look for early enhancement, enhancement along ducts, or areas of irregular enhancement, Mendel said. CT can't perform as thoroughly as a full kinetic MRI study with five to seven phases, he said, but with contrast it's usually sensitive enough to find out what's going on in the breast.
Remember to look at the breast in CT data, and use it for problem solving, he said. "If you don't think about breast CT, you're not going to see the incidental lesion, and you're not going to be able to use it for intervention."
By Eric Barnes
AuntMinnie.com staff writer
July 11, 2007
Related Reading
German group presents results with prototype breast CT scanner, March 11, 2007
Koning introduces CT for breast imaging, November 26, 2006
Imaging start-up to install conebeam CT breast imaging prototype, May 1, 2006
Breast CT developers aim to 'revolutionize' mammography, December 20, 2005
Researchers make inroads with breast CT, gear up for clinical test, July 25, 2005
Copyright © 2007 AuntMinnie.com