Liver-Spleen Imaging
Radiopharmaceuticals & Technique:
Tc-sulfur colloid: (Dose: 5mCi)
Average particle size is between 0.1 to 1 micron. Gelatin is added to prevent further growth of the particles. The preparation should not be used if it is over 6 hours old due to particle agglomeration.
The sulfur colloid particles are phagocytized by the reticuloendothelial cells with an extraction efficiency of 95%. Blood clearance half-time is about 2 to 3 minutes. The particles are fixed intracellularly for an indefinite period of time. Particle size is an important determinant of their distribution. Particles between 0.3 and 1.0 microns are predominantly phagocytized by the Kupffer cells of the liver. Small particles (less than 0.1 micron) distribute primarily to the bone marrow. Particles larger than 1 micron distribute mostly to the spleen, while very large particles will be deposited in the lungs.
Uptake of the tracer reflects distribution of hepatic perfusion and functioning reticuloendothelial cells in the liver (Kupffer cells) & spleen. Although Kupffer cells make up less than 10% of the liver cell mass, they are distributed uniformly throughout the liver. The normal distribution is to the liver (80-90%), spleen (10%), and bone marrow (5%). Increased bone marrow activity can be seen with hemolytic anemias.
Tc-Albumin colloid
Unlike sulfur colloid particles which remain fixed in the RE system, albumin colloid particles are metabolized and cleared.
Hepatic Disease
Scintigraphic Patterns
- Budd-Chiari (Hepatic vein thrombosis): Caudate lobe (posterior)
- SVC obstruction: Quadrate (anterior)
- Hemangioma
- Focal nodular hyperplasia
- Cirrhosis (Regenerating nodules)
- Cirrhosis/Severe hepatocellular dysfunction
- Faulty colloid preparation with excess aluminum: Results in large colloidal particles
- DIC/Bacterial endotoxin
- Estrogen therapy
- Widespread pulmonary metastases
- Amyloidosis
- Histiocytosis X
- Pulmonary Infection/Trauma (focal)
- Neoplasm (focal)
- Met (esp. colon or if mult.)
- Cyst
- Hepatoma (esp. if assoc. cirrhosis)
- Hematoma
- Hemangioma
- Abscess
- Pseudotumor (Cirrhosis)
Colloid Shift:
With a loss of functioning hepatic parenchyma (or liver blood flow) a "shift" in phagocytic function will result in enhanced colloid uptake by other reticuloendothelial tissue, especially the spleen and bone marrow. In severe hepatic failure, uptake in the lungs may occur. A spleen to liver ratio of greater than 2:1 is considered evidence of colloid shift [Zeisman quotes greater than 1.5:1 as abnormal]. Colloid shift is a non-specific finding and may be due to hepatocellular dysfunction (cirrhosis, passive congestion, chemotherapy), infection (hepatitis, mononucleosis, sepsis), or marrow activation. Some authors differentiate colloid shift (prominent splenic and bone marrow activity) from simple shift (reversal of the normal liver to spleen ratio).
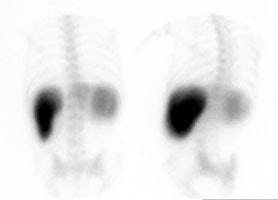
Colloid shift: A posterior and posterior oblique image from a Tc-SC exam demonstrate markedly increased splenic activity in association with an enlarged spleen. The liver is small and bone marrow activity can also be seen. The extrahepatic reticuloendothelial accumulation of the tracer indicates hepatocellular dysfunction. |
|
Focal Hepatic Hot Spot:
In the presence of SVC or innominate vein obstruction a bolus injected into the basilic vein can travel via collaterals and deliver a large amount of activity to the anterior mid portion of the liver (quadrate lobe- inferior portion of the medial segment of the left lobe [segment IV]) [1]. The collateral venous pathway is via the internal mammary vein to recanalized umbilical vessels that connect to the left portal vein [1]. This may have the appearance of gallbladder activity. Injection in the foot will result in a normal scan.
DDx of focal "hot spot"
Diffuse Lung Activity:
Pulmonary uptake is felt to involve activation of pulmonary macrophages, RE cell migration from other parts of the body to the lungs, or an alteration in pulmonary endothelium.
DDx of Diffuse Lung Activity
Solitary Cold Lesion:
EtOH Associated Liver Disease
Early in the disease course the liver may be normal or enlarged with diffusely decreased activity due to alcoholic hepatitis or fatty infiltration. A mottled pattern- due to recurrent injury, scarring, and regeneration, can also be seen. Colloid shift and splenomegaly are typically noted. If ascites is present there will be displacement of the right lobe from lateral abdominal wall and diaphragm, and indistinctness of liver margin. The right lobe is frequently more affected by the process and as the disease progresses it will become smaller due to parenchymal scarring. The left lobe will appear relatively enlarged as a result. In cirrhosis colloid shift is felt to be secondary to intrahepatic shunting as the scan often fails to become normal even after the portal hypertension is alleviated. The amount of colloid shift to the spleen, however, is not a reflection of the degree or presence of portal hypertension.
Budd-Chiari Syndrome (Hepatic Vein Thrombosis)
Patients with Budd-Chiari typically present with hepatomegaly (due to congestion) and ascites.
Etiologies of Budd-Chiari syndrome include:
- Tumor vascular invasion
- Hypercoaguable states
- Idiopathic causes
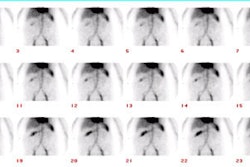
Scintigraphic findings early in the disorder are characterized by a diffusely mottled tracer uptake in the liver. Over time this will progress to diffusely decreased activity. The caudate lobe will usually enlarge and show relatively increased activity as a result of its separate venous drainage directly into the IVC. If inferior vena caval obstruction is present, the scan will show diffuse hepatocellular dysfunction.
Diffuse and Infiltrative Disorders
**These disorders frequently result in decreased hepatic pliability and hepatomegaly (normally liver measures 17-18cm on the anterior view). Scans may also reveal diffusely decreased activity, as well as focal defects.
Etiologies of diffusely diminished hepatic activity include:
- Normal variant (large pt)
- Hemochromatosis
- Diffuse hepatocellular dz (Hepatitis)
- Fatty infiltration
- Mets (Infiltrative mets, such as lung or breast, produce a coarse inhomogeneous pattern)
- Lymphoma
- Amyloidosis
Trauma
Since the advent of CT scanning, this procedure is rarely performed in the setting of acute trauma. A subcapsular hematoma will create a peripheral impression on the margin of the liver. Localized hemorrhage can produce a intrahepatic defect.
Metastatic Disease
At present the use of Tc-SC imaging for metastatic disease is minimal. It had a reported sensitivity of 90-95% for SPECT imaging, with a lower specificity. The exam is limited due to it's inability to detect small (less than 1cm) lesions.
Splenic Disease
General findings
On colloid imaging, the activity in the spleen is typically equal to or less than that of the liver. The spleen normally measures about 10 cm in length (+/- 2 cm), but there is tremendous variability particularly based upon patient size. In children, normal splenic size may be estimated by the formula L= 5.7 + 0.31 A (where A is the child's age in years). Some normal splenic variants include: The "upside down spleen" in which the splenic hilum presents on the upper margin as a concave defect producing a crescent appearence. A splenic lobule is a small appendage of normally functioning splenic tissue adjacent (usually anterior or inferior) to the spleen.
Focal splenic lesions or defects
- Infarction: The defect produced by infarction is typically wedge shaped and peripheral. Splenic infarcts are associated with bacterial endocarditis (50% of cases), sickle cell, myeloproliferative disorders, and infiltrative disorders such as Gaucher disease.
- Neoplasm: Mets, lymphoma, melanoma, sarcoma, chorioepithelioma
- Abscess
- Hematoma
- Cyst
Splenic Trauma:
Rupture
- Appears as a linear or stellate defect within the parenchyma
- Intrasplenic- localized defects
- Subcapsular- semilunar/thumbprint indentations
- Large hematomas may displace the spleen
- Following trauma, splenic tissue may seed other locations (autotransplantation) such as other abdominal or pelvic viscera, the diaphragm, or lungs.
Hematoma:
Splenosis:
Accessory Spleens:
Most commonly located near the splenic hilum. These are often small and missed on TcSC imaging, but will frequently hypertrophy following splenectomy. Accessory spleens are detected in approximately 10 to 30% of patients following splenectomy. Shielding of liver activity is essential when trying to identify sites of residual splenic tissue in post splenectomy patients on Tc-SC imaging.
Heat damaged or denatured Tc-RBC's can also be used to detect multiple or accessory spleens, or to define the presence of asplenia. The patient's own RBC's are withdrawn and labeled in an in vitro manner. They are then incubated in a 50 degree Celsius water bath for 15 minutes and readministered to the patient. Masking the liver will help in detecting small amounts of activity.
Non-visualization of the Spleen:
- Congenital asplenia: Associated with cardiac & GI abnormalities
- Sickle cell- autosplenectomy
- Post-op/Traumatic avulsion/Infarct
- Graft vs. Host Disease
- SLE
- Tumor infiltration
Other Tc-SC imaging:
Renal Transplant:
Normally, less than 0.2% of the administered Tc-colloid dose is excreted by the kidneys. Renal allografts undergoing rejection demonstrate marked increased accumulation of the tracer. The radionuclide is trapped in fibrin thromboses deposited in the allograft vasculature. Renal allograft accumulation of sulfur colloid has also been described in cyclosporin induced hemolytic uremic syndrome.
Peritoneovenous Shunt Patency:
Peritoneovenous shunting can be used in the treatment of intractable ascites. The afferent limb of the shunt is a silicone tube which is placed intraperitoneally. This is connected by another tube which is tunneled over the chest wall into the superior vena cava. Respiratory pressure changes permit fluid to flow into the venous system. Malfunction occurs in 15-20% of shunts and is most frequently related to fibrin clots in the afferent limb. Thrombosis of the efferent catheter near the SVC occurs less frequently.
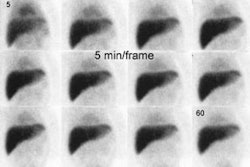
Intraperitoneal injection of Tc-MAA (or Tc-SC) can be used to assess shunt patency. Visualization of the venous portion of the shunt and lungs indicates shunt patency (generally by 25 minutes of the exam). There may be non-visualization of the efferent limb of the shunt, but as long as lung activity is seen, shunt patency can be assumed. Non-visualization of pulmonary activity is indicative of shunt malfunction. To locate the site of malfunction, 2.0 mCi of Tc-MAA can be injected directly into the efferent tubing. If activity moves into the lungs, then the problem is in the afferent limb or valve. Congestive heart failure with elevated right heart pressure can produce a false positive exam.
REFERENCES:
(1) Radiology 2005; Dickson AM. The focal hepatic hot spot sign. 237: 647-648