Radionuclides
Iodine-123
I-123 decays by electron capture, has a physical half-life of 13.6 hours, and a gamma energy of 159 keV. It is produced in a cyclotron by either one of two methods:
I-127(p,5n) Xe 123 -> I 123
This method requires more energy, but produces I-123 of higher purity with no I-124 contamination and very little I-125 (I-125 has a half-life 60 days and emits 25 to 35 keV x-rays which contribute significantly to the radiation exposure to the patient). Because I-123 decays much faster than these contaminants, doses which are more than 24 hours old should not be used.
Te-124 (p,2n) I-123
This method results in impurities such as I-124 (5%), I-125, I-126, and Na-24. The I-124 has higher energy gamma emissions and a 4.2 day half-life which contribute to image degradation and patient dose, respectively.
Dose
200-400 uCi
Indications
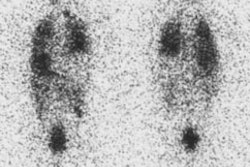
I-123 is the agent of choice when evaluating substernal goiters because there is usually substantial mediastinal blood pool activity associated with Tc-pertechnetate. The maximal count rate in the thyroid occurs approximately 6 hours following the oral administration of the agent. Images are typically acquired 4 hours following administration of the tracer, and uptake values are determined at 4 and 24 hours.
Iodine-131
Iodine-125
I-125 is not used for imaging. The agent decays by electron capture with a physical half-life of 60.2 days. It emits a gamma photon of 35 keV. The agent is primarily used for radioimmunoassays and other in vitro procedures.
Technetium-99m Pertechnetate
- Patient has been taking thyroid blocking agents (Propylthiouracil). Thiouracil blocks oxidation and organification of iodide following its uptake by the thyroid gland, but will not interfere with trapping of pertechnetate.
- Patient is unable to take medication orally
- The study must be completed in < 2 hrs
- thyroid function (uptake studies) are not necessary
Pertechnetate (TcO4-) is a monovalent anion trapped by the thyroid gland in the same manner as iodine (an active transport mechanism). After trapping pertechnetate slowly "washes" from the gland- it does NOT undergo organification. Peak thyroid activity occurs between 20 and 40 minutes after injection. Only 2-4% of the administered dose is trapped in the thyroid. Pertechnetate is secreted in human milk (discontinue breast feeding for 48 hours after dosing) and also crosses the placenta to accumulate in the fetus.
Iodine and pertechnetate share the same active transport uptake pathway. The uptakes of radioiodine and pertecnetate by the follicular trapping system are both decreased by perchlorate, thiocyanate ions, and expansion of the circulating iodide pool (iodinated contrast, dietary, or the antiarrhythmic agent amiodarone).
The typical dose used for thyroid imaging is 3 mCi intravenously.
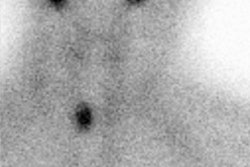
Dr. Fink-Bennet feels that a rough estimate of thyroid uptake can be obtained from the Tc-pertechnetate exam by obtaining a 1 minute anterior planar image over the thyroid and salivary glands 5 minutes after injection of the tracer. A hypofunctioning gland will appear less intense than the salivary glands, a normal gland equal to the salivary glands, and a hyperfunctioning thyroid hotter than the salivary glands.
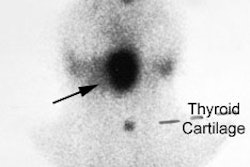
In comparison to I-123 studies, more background activity is usually present on pertechnetate images. Linear esophageal activity, due to tracer secreted by the salivary glands which is swallowed, may be seen. This can be cleared from the esophagus by drinking water. (Note: See Pyramidal Lobe below). A pinhole collimator is used for enhanced resolution and also facilitates oblique views.
The size of nodules that can be detected by pertechnetate imaging depends upon the nodules function and size. Hot nodules may be seen even if they are very small, but a hypofunctioning nodule less than 0.8 to 1.0 cm in size lying within the gland may not be discernible. In general, Tc-pertechnetate 5-mm pinhole imaging has a sensitivity of 80 to 95% for cold nodules between 8 to 18 mm, but nearly 0% for nodules less than 5 mm. There are reported cases of thyroid carcinomas that are capable of trapping but not organifying iodine. Therefore, it is possible to have a warm or hot nodule on a Tc-99m scan that would be cold on I-123. Therefore, any patient with a non cold nodule on a Tc-99m scan should be repeated with I-123 to avoid this disparity. Cold nodules with Tc-99m scan will inevitably be cold with an I-123 scan.
Pertechnetate is the preferred imaging agent when:
Radiation dose to the thyroid, by agent
Assuming normal sized adult gland (20 gm) with normal RAIU (15%):
* I-131: 800-1000 rad/mCi; 16,000 rad/mCi in the neonate
* I-123: 7.5 rad/mCi (adult); 160 rad/mCi (neonate)
* I-125: 450 rad/mCi
* 99mTc-O4: 0.13 rad/mCi (adult); 3.4 rad/mCi (neonate)