Imaging Findings in Thallium Exam
Normal Variants
Mild decreased activity is commonly seen in association with:
Apical thinning
Normal apical thinning subtends an arc of less than 30 degrees. The defect is usually symmetric about the apex and there is no redistribution.
Basal segments
Due to diaphragmatic attenuation. Attenuation correction programs can be used to decrease this problem, however, they often overcorrect and can decrease the sensitivity of the exam to identify true inferior/basal ischemia [33].
Upper septal area
The membranous septum typically has little or no activity compared to the muscular septum.
Right ventricular activity
RV activity can be seen during exercise, but should be noted only faintly at rest. RV activity on rest images is associated with right ventricular pressure overload (>30mmHg), volume overload, or both. In patients with pulmonary arterial hypertension, development of right ventricular enlargement and dysfunction (cor pulmonale) is associated with poor survival. When pulmonary artery pressure is raised the right ventricle is susceptible to ischemia due to limited coronary reserve for the hypertrophied ventricle. Patients with pulmonary hypertension have greater right ventricular thallium uptake after dipyridamole stress which increases with increasing myocardial mass. Patients with the most RV uptake have the most significant impairment of RV systolic function, independent of ischemia [1].
Another finding associated with RV hypertrophy is loss of the interventricular septum's normal convexity into the right ventricle. Isolated right ventricular volume overload produces dilatation of the RV with maintenance of septal convexity toward the right ventricle. It can occur secondary to an ASD, VSD, or tricuspid regurge.
Increased Pulmonary Activity
Pulmonary activity is an indicator of left ventricular end-diastolic pressure. The amount of pulmonary activity is dependent upon the heart rate obtained. If an individual failed to achieve adequate cardiac stress one would expect a greater amount of pulmonary activity. In general, in an adequately stressed patient, pulmonary activity should be less than 50% of cardiac activity (Heart to lung activity ratio greater than 2:1). Increased lung activity is seen in association with:
1. Marked exercise induced left ventricular dysfunction. Increased pulmonary activity is felt to reflect pulmonary edema secondary to transient global LV dysfunction. It may be the only evidence of 3-vessel disease (global ischemia).
2. Pulmonary venous hypertension (Mitral valve disease).
Increased pulmonary activity is associated with a markedly increased risk of future cardiac events. An abnormal heart to lung ratio is a poor prognostic indicator and is perhaps the most important prognostic indicator for the likelihood of future cardiac events [2]. The positive predictive value of increased lung uptake for subsequent cardiac event is approximately 70% (the negative predictive value is 86%).
As with exercise thallium imaging, increased pulmonary activity on dipyridamole stress exams may be a marker of functionally more significant coronary artery disease. Myocardial to background ratios are comparable in both exercise and dipyridamole imaging, most likely due to a relatively greater myocardial uptake of the tracer with pharmacologic stress. Although dipyridamole should not induce ischemia, perhaps there is vasodilator induced subendocardial hypoperfusion as a result of a "steal phenomenon" which results in LV dysfunction [3].
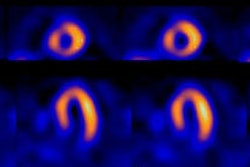
Dilatation of the left ventricle with stress
Scintigraphic evidence of left ventricular dilatation with stress indicates significant left ventricular dysfunction (ie: ischemia may be more extensive than indicated by perfusion defects alone). There is a strong correlation (sensitivity 60%, specificity 95%) between LV stress dilatation and the presence of multivessel CAD (often with critical stenoses). Stress induced left ventricular dilatation is also a poor prognostic indicator [4].
Dilatation is less likely to be noted on images performed with Tc-Sestamibi due to the delay prior to imaging. If it is seen, it most likely represents the presence of subendocardial ischemia and not transient ischemic chamber dilatation due to the lack of redistribution of the agent (ie: it provides a snap-shot of perfusion at the time of injection).
Stress dilatation can also be identified with dual-isotope (thallium/sestamibi) imaging. A left ventricular endocardial volume stress to rest ratio of greater than 1.22 has been shown to be a sensitive (71-77%) and specific (92-95%) indicator of severe and extensive coronary artery disease [23]. The ratio is determined by automated quantitative software and this measured ratio is more accurate than visual analysis [23].
Other causes of transient dilatation of the left ventricle with stress in the absence of coronary artery disease include: 1- Severe hypertensive heart disease: Due to subendocardial ischemia associated with delayed diastolic left ventricular relaxation, decreased capillary density in the hypertrophied myocardium, and elevated end-diastolic pressures [21]; and 2- Dilated cardiomyopathy: Due to limited coronary flow reserve [21].
Myocardial Viability
It has been estimated that between 25-40% of patients with chronic coronary artery disease and left venticular dysfunction have the potential for significant improvement in left ventriular function following revascularization [30]. In patients with LVEF's below 30%, coronary revascularization can improve LV function, heart failure symptoms, and long term prognosis when compared to medical treatment alone [25,30]. Patients with ejections fractions greater than 50% have a 4-year survival rate of 92%, compared to only 57% for those with ejection fractions below 35% [34]. Unfortunately, patients with reduced LVEF's are at a greater risk for surgical mortality from CABG (about 4% mortality) and physicians are reluctant to recommend surgery if the prospects for benefit are limited. Because post-operative improvement in LVEF has been related to the preoperative identification of viable myocardial tissue, viability is a crucial factor when considering chronic CHF patients for coronary artery bypass grafting [30]. Patients with a greater percentage of viable tissue are more likely to have improved LVEF and symptoms [25]. Although restoration of myocardial function is unlikely in the absence of viable tissue, revascularization can be associated with other benefits such as pain relief and decreased incidence of arrhythmias. Immediately following revascularization there may be a period of stunning in which LV function deteriorates. Imaging 2 to 3 months after the procedure is probably more representative of true post-op LV function. Improvement in regional function may occur without improvement in overall ejection fraction. LV size is also an important determinant of the potential for recovery of function- little to no improvement is seen in patients with marked LV dilatation [5].
Stunned myocardium
Stunned myocardium refers to myocardial contractile dysfunction that follows a period of coronary occlusion even after flow has been restored to an area that has no irreversible damage. It represents the combined results of ischemic and reperfusion injury. Stunning represents a flow-contraction mismatch that is typically seen in the clinical setting of thrombolytic therapy for acute myocardial infarction. Stunning has also been described in the recovery phase after exercise induced ischemia, in the post-operative CABG period, in the setting of unstable angina, and following coronary angioplasty [6].
In the classical setting, stunning may persist for days up to 8 weeks after revascularization [1], but generally improvement in regional wall motion is seen after 2 to 3 weeks without further intervention. Proposed mechanisms for the observed wall motion abnormalities include: 1- Abnormal energy utilization by myofibrils, 2- Production of cytotoxic oxygen free radicals, 3- Altered calcium flux, and 4- Accumulation of neutrophils in previously ischemic tissue. As there is restored flow to this area with viable myocardial cells, areas of stunned myocardium will accumulate Thallium (or Tc-Sestamibi), but will demonstrate a wall motion abnormality on gated imaging studies.
Despite the close correlation between thallium uptake after reperfusion and subsequent improvement in regional wall motion, early post-reperfusion thallium uptake appears to overestimate myocardial viability. This may occur because in the period soon after reperfusion, the distribution of thallium may reflect hyperemic flow, thereby overestimating the extent of myocardial salvage. Thus, early thallium uptake after reperfusion cannot reliably differentiate viable from necrotic myocardium. However, necrotic myocardium cannot retain thallium and despite its initial uptake, thallium washout is accelerated from these areas. (See Reverse Redistribution)
Dobutamine echocardiography has been reported to identify stunned myocardium by demonstrating improvement in myocardial thickening and regional wall motion compared to a baseline exam.
Hibernating myocardium
Hibernating myocardium represents severely ischemic, but viable myocardial tissue. There is a chronic reduction in myocardial metabolism/ contractility in order to match a long-standing decrease in blood supply (chronic ischemia). In other words, the cells maintain viability, but cannot perform mechanical work [20]. This may be a protective response by the myocytes to reduce their oxygen demand in the setting of reduced oxygen availability. This is a reversible phenomenon and ventricular dysfunction can improve if flow is restored. Because enhanced left ventricular function after revascularization is associated with improved survival, it is crucial to identify areas of viable myocardial tissue. For a discussion of thallium imaging in the detection of hibernating myocardium see "Rest-Redistribution Thallium Imaging".
Sestamibi Imaging of Hibernating Myocardium
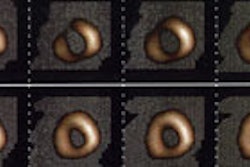
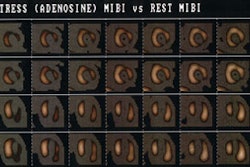
Thallium reinjection is superior to Tc-Sestamibi imaging in identifying viable myocardium in patients with chronic coronary artery disease [7]. Since the primary determinant of Tc-MIBI uptake is regional coronary blood flow rather than tissue viability, Tc-Sestamibi can underestimate the presence of viable myocardium in states of greatly reduced perfusion. Approximately 35 to 60% of reversible myocardial regions on Thallium reinjection imaging will appear as fixed defects on exercise-rest images with Tc-Sestamibi [7,8]. Even if defect severity is taken into account, Tc-Sestamibi studies are likely to prove ineffective in separating subendocardial infarction from hibernating myocardium [9].
Nonetheless, Dilsizian found that moderate reduction of Tc-sestamibi activity (51 to 85% of normal) in a fixed defect is more suggestive of viable myocardium and by applying this standard the concordance between thallium and Tc-sestamibi studies increases to 93%. He also found that by performing a 4 hour redistribution image with Tc-sestamibi prior to stress imaging, 38% of defects which appeared fixed on the rest/stress exam demonstrated increased activity indicating viability. This increased the thallium-sestamibi concordance to 82% (unfortunately, sestamibi still falsely identified 18% of reversible defects as fixed).
Other researchers have found similar results by evaluating the severity of the perfusion defect on Tc-Sestamibi images. Uptake within a defect of over 60% of the maximum cardiac activity is associated with a 70% likelihood of improved regional wall motion after revascularization. Regions with uptake less than 60% have very little likelihood of demonstrating improved wall motion after revascularization [DePuey, Harvard Course, 94]. In another study based upon comparison with FDG imaging, Tc-sestamibi uptake of less than 30% of the peak myocardial activity had a predictive value of over 80% that this area represented a scar. Unfortunately, between 25 and 50% of segments with defects of 41 to 60% of peak uptake were shown to be viable on FDG imaging, respectively. Segments with severe Tc-sestamibi defects with preserved FDG uptake were associated with severe hypokinesis on wall motion studies [10].
Other apparently successful attempts to improve the detection of viable myocardial tissue with Tc- MIBI include rest sestamibi exams performed following the administration of nitrates (most likely the result of the vasodilatory effects of the nitrates) [11,12] and delayed redistribution cardiac imaging after resting Tc-MIBI injection. Such delayed images have revealed improved uptake of tracer in 24 to 38% of rest defects [13,14].
Despite these efforts to demonstrate the value of Tc-Sestamibi, it must be remembered that reinjection thallium imaging (as discussed above) provides information regarding myocardial viability similar to that of PET imaging. The concordance between the two techniques regarding the presence of viable or nonviable myocardium is about 90%.
FDG PET Imaging of Hibernating Myocardium
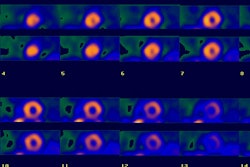
FDG-SPECT imaging can also be used to assess for the presence of hibernating myocardium [15]. In the fasting state, fatty acids are the primary fuel for producing high energy phosphate (ATP) in the normal myocardium. The breakdown of fatty acids via beta-oxidation in the mitochondria, however, is very sensitive to oxygen deprivation. During periods of ischemia or hypoxia the myocyte compensates for the loss of oxidative potential by shifting toward glucose utilization to generate high energy phosphates. The amount of energy produced via glycolysis may not be sufficient to sustain mechanical work, but is adequate to maintain cell viability. Glycolysis can only be maintained if lactate and hydrogen ions (the byproducts of glycolysis) do not accumulate intracellularly. Therefore, blood flow must be sufficient to deliver glucose to the cell and remove the metabolites of the glycolytic pathway. Once perfusion is decreased below a critical level, the tissue concentrations of lactate and hydrogen ions will increase and inhibit glycolysis [30]. This results in a loss of ion concentration gradients across the cell membrane, followed by cell membrane disruption, and cell death [30].
As previously noted, flow images of regions of hibernating myocardium will demonstrate markedly diminished perfusion. However, because areas of hibernating myocardium have a shift towards greater glucose utilization as a metabolic substrate, FDG PET scanning will demonstrate enhanced uptake of the tracer in the regions of diminished perfusion. This is refered to as a "FDG-Blood flow mismatch." Scar tissue will demonstrate a concordant reduction in perfusion and FDG uptake (a FDG-perfusion match") [30].
FDG PET imaging is considered the standard of reference for detecting hibernating myocardium [20]. As previously mentioned, up to 40-50% of fixed thallium defects on non-reinjection images have been shown to be viable on FDG imaging. Improved contractile function is identified in 80-85% of such regions following revascularization (EF improved an average of 15%), but in only 10-20% of regions which fail to demonstrate metabolic activity. For the prediction of regional wall motion improvement following revascularization, FDG PET has a mean sensitivity of 88% and a mean specificity of 73% [29]. The positive and negative predictive values for predicting functional improvement after revascularization with FDG PET imaging are 76% and 86-92%, respectively [20,29]. When 25% of more of the LV was viable, a significant improvement in LVEF can be expected [29].
MR Imaging for Hibernating Myocardium:
MR imaging is also being studied for the assessment of myocardial viability [34]. Because of the excellent anatomic resolution that can be achieved with rapid cardiac imaging sequences, MR determination of viability is based upon visible changes in myocardial wall thickeness [34]. Six to eight short axis sections can be obtained and images reviewed in cine format [34]. Hypokinetic or akinetic segements demonstrate less than 1 mm of wall thickening [34]. Normal myocardial tissue has an end-diastolic wall thickeness greater than 5.5 mm and systolic wall thickening greater than 1.5 mm [34]. Hibernating myocardium has an end-diastolic wall thickenss greater than 5.5 mm and wall thickening less than 1.5 mm [34]. Infarcted myocardium has an end-diastolic wall thickness less than 5.5 mm and wall thickening less than 1.5 mm [34]. Patients with acute myocardial infarctions less than 3 weeks old should not be evaluated for viability as areas of stunned myocardium may not have regained full function and the areas of infarcted myocardium may not have had time to allow the scarring process to produce wall thinning [34]. MR has a sensitivity of between 55% in predicting improvement in function in a myocardial segment after revascularization [34]. Segments felt to be representative of hibernating myocardium that failed to demonstrate improved function were commonly adjacent to infarcted segments or had nontransmural wall thinning [34]. The lack of improved function in regions adjacent to areas of infarcted myocardium may be related to mechanical tethering [34]. Also, myocardium adjacent to areas of chronic infarction have hypertrophied myocytes that have impaired contractile function [34]. In regions where wall thickness is greater than 5.5 mm, but less than normal, there is a reduction in muscle mass and the amount of recovery can be reduced. A subendocardial infarct with some preserved EDWT may limit improvement in left ventricular function [34].
Reverse Redistribution
Reverse redistribution does not indicate ischemia [2]. It is present when the initial post exercise images are either normal or show a perfusion defect and this defect appears larger on delayed images [2]. In other words, regions which demonstrate reverse redistribution have activity which appears similar to adjacent regions on the initial scan which indicates a non-critical stenosis in the supplying artery or adequate collateral circulation. These areas, however, demonstrate a more rapid clearance of thallium than normal which is felt to be related to an inability of the myocytes in these regions to retain thallium (ie: less than a full complement of normal functioning myocytes), and initial thallium uptake within non-viable myocardium and the interstitial space. Reverse redistribution can be seen with both stress-redistribution and rest-redistribution imaging (see discussion in Rest-Redistribution imaging section).
This pattern has been most commonly observed in patients who have had an acute myocardial infarction and have undergone treatment with coronary thrombolysis or another form of revascularization [2]. In this setting, reverse-redistribution is frequently associated with patency of the infarct related artery, non-transmural infarction, and relatively normal wall motion in the affected region [16]. In the post-revascularization period there is a mixture of scar and stunned myocardium which probably results in the poor retention of tracer. Thus, early after reperfusion, reverse redistribution may be seen as evidence of infarct-related artery patency and has a better prognosis than the classic reversible defect. It has also been described soon after angioplasty or bypass surgery, again in the presence of a patent graft or supplying artery. In patients with known chronic CAD, this finding may represent the presence of scar within a segment containing viable myocardial elements- whether normal, stunned, or hibernating. [17]
In the general population, reverse redistribution has been found to be associated with coronary artery disease. Frequently such segments are supplied by occluded epicardial vessels (50% of cases), with good collateral circulation (seen in 60%). These segments are also noted to have abnormal wall motion. Reverse redistribution has also been described in a variety of cardiomyopathies including sarcoidosis and Chagas' disease. It is important to remember, however, that in patients with a low pretest likelihood of disease, this finding can represent normal variability in the clearance of thallium or an imaging artifact.
Preliminary observations from the Thrombolysis and Myocardial Infarction trial suggest that reverse-redistribution is associated with a higher incidence of future cardiac events independent of the presence of ischemia. Such events (defined as unstable angina or acute MI) occurred in 30% of patients- particularly those with severe reverse-redistribution. About three-quarters of segments with reverse-redistribution are viable by PET FDG imaging and viable segments generally demonstrate normal wall motion on the MUGA exam. Segments with wall motion abnormalities have over a 50% chance of representing scar [18].
In the setting of revascularization following an acute myocardial infarction, reverse-redistribution can also be seen on technetium agent imaging if delayed images are performed [32]. Mitochondrial membrane potential alterations likely occur following a period of ischemia and revascularization [32]. This alteration contributes to a decreased capacity to retain technetium perfusion agents [32]. None-the-less, delayed images are typically not acquired when using these agents.
False Positive Thallium Exam
(Reversible or Fixed Perfusion Defects in the Absence of Coronary Artery Disease at Coronary Angiography)
Reversible perfusion defects have been reported in up to 27% of selected patients with angina and normal findings on coronary angiography [24].
NOTE: The accuracy of myocardial perfusion scintigraphy has previously been evaluated using coronary angiography as the gold standard. Angiography is a silhouette technique with substantial limitations [24]. Recent work with intracoronary sonography indicates that coronary angiography can underestimate the extent and severity of coronary artery disease- particularly in the early stages of atherosclerosis [24]. Reversible perfusion defects on myocardial perfusion scintigraphy associated with normal coronary angiography may actually represent occult, unrecognized atherosclerotic coronary artery disease which is commonly associated with an abnormal vasodilatory capacity [24].
1. Normal variant
a- Diaphragmatic attenuation
Produces a fixed inferior perfusion defect. It can be exaggerated in obesity and with a full stomach. Prone positioning can reduce diaphragmatic attenuation, but may create an anterior wall defect.
b- Breast shadow or breast implant
The breast artifact is most easily appreciated on the rotating tomographic projection or volume rendered images, but can also be seen on planar images. The degree of attenuation varies directly with breast size and tissue density. Classically these defects produce fixed anterior or lateral wall defects, however, any wall can be involved. Remember- body builders with heavily muscled pectoralis muscles have also produced this artifact.
c- Pacemakers
Although pacemakers are implanted above and below the diaphragm, it is unusual for a pacemaker to intrude into the chest image and interfere with image interpretation.
2. Mitral Valve Prolapse
Exercise perfusion defects are uncommon (less than 5%) in patients with mitral valve prolapse, but may be related to exercise induced stimulation of sympathetic activity. This activity produces a tachycardia which will increase the degree of prolapse and consequently stretch the cordae tendinae on the papillary muscles. This stretching may cause ischemia of the papillary muscles and surrounding myocardium. This is only theory, however, and the actual mechanism for these defects is unknown. Since this phenomenon is uncommon, reversible defects in patients with prolapse should still be considered ischemia until proven otherwise. [19]
3. Valvular Heart Disease
a. Mitral Regurgitation
b. Aortic Stenosis:
Between 40 to 60% of patients without significant coronary lesions demonstrate either fixed or reversible defects which are probably related to a decreased perfusion gradient in the coronary arteries associated with a tight aortic stenosis and/or the severity of the left ventricular hypertrophy. These perfusion abnormalities may improve postoperatively following the relief of stresses on the pressure loaded ventricle.
c. Aortic Regurgitation:
Patients with aortic regurgitation may demonstrate reversible stress apical defects in the absence of coronary artery disease. With eccentric hypertrophy, the perfusion pressure to the "watershed areas" between the coronary vessels decreases to yield apparent perfusion defects. Perfusion defects elsewhere, should be considered indicative of CAD until proven otherwise.
4. Left Bundle Branch Block
In left bundle branch block (LBBB), there is delayed septal activation and relaxation which adversely affects diastolic coronary flow regionally. With exercise, the myocardium experiences decreased diastolic perfusion time which yields decreased radiotracer extraction by the septum relative to the lateral wall. Thus, these patients may have a reversible septal/anteroseptal defect that is most pronounced at high heart rates. This defect should NOTinvolve the apex. When it does, this favors a diagnosis of ischemia. Pharmacologic stress with dipyridamole or adenosine which do not increase the heart rate significantly (and therefore should not affect diastolic flow) can be useful in these patients. Dobutamine stress, which increases heart rate, can produce this artifact (JNM, Dec.94).
5. Idiopathic Hypertrophic Subaortic Stenosis
Increased count density in the region of the thickened septum results in an apparent relative decreased activity in the lateral wall which leads to the impression of a fixed defect in this location. Myocardial perfusion imaging may not be able to reliably distinguish CAD in these patients. Nonetheless, the presence of any type of thallium abnormality in these patients is strongly associated with potentially lethal arrhythmias. (Nucl Med Annual 93, p.214)
6. Hypertensive Myocardial Hypertrophy
Despite concentric myocardial hypertrophy in these patients, there is often increased septal radiotracer activity relative to the lateral wall on both stress and rest images. This increased count density leads to a relative decreased count density in the lateral wall, which may be misinterpreted as a fixed lateral wall abnormality.
7. Cardiac contusion
8. Infiltrating myocardial disease
Sarcoid, Amyloid, Neoplasm
9. Cardiomyopathy
a. Dilated Cardiomyopathy
b. Hypertrophic Cardiomyopathy:
Ischemia is probably related to an imbalance between oxygen supply in face of the increased myocardial mass, septal perforator arterial compression, abnormalities of intramural arteries, and disturbance of left ventricular relaxation.
10. Bland-White-Garland Syndrome
(Anomalous origin of the left coronary artery from the pulmonary artery)
This anomaly most commonly results in death during early infancy, but survival into adulthood can occur if collateral coronary flow is sufficient. Patients are generally noted to have an anterior wall ischemic perfusion defect. An inferior/posterior perfusion defect may also be seen secondary to a right coronary artery to left coronary artery to pulmonary artery shunt.
11. Coronary spasm
Coronary artery spasm occurs in angiographically normal coronary artery vessels or superimposed on obstructive coronary artery disease. Patients with Prinzmetal's angina, cocaine overdoses, and collagen vascular diseases like scleroderma are known to have perfusion defects despite normal coronary arteriograms. Provocative testing with ergonovine during cardiac catheterization may demonstrate latent coronary artery spasm.
12. Myocardial bridge
Myocardial bridging is a rare angiographic finding (<1% ). Since the LCX and RCA follow the AV groove, myocardial bridging is almost exclusively seen with the LAD. The coronary artery dips below the epicardium and runs within the myocardium for a short distance. The characteristic angiographic finding is systolic narrowing of the LAD that disappears during diastole. Myocardial bridging that produces a 75% or greater systolic stenosis can demonstrate reversible perfusion defects. Lesser degrees of narrowing are generally not associated with perfusion abnormalities. (Annual 93, p.209)
13. Myocarditis
14. Decreased coronary flow reserve: Syndrome X
Syndrome X is defined as stress-induced anginal pain with a positive stress test for myocardial ischemia, normal findings on coronary angiography, and normal left ventricular function. This is considered a "small vessel disease" syndrome with a reduced coronary vasodilatative reserve of the coronary microcirculation. Its etiology is unclear but may be due to a variable response to exercise and/or pharmacologic stress by the coronary vessels (some dilate more than others) creating an apparent defect. [22]
15. Recent Post-PTCA
Post PTCA scans should be delayed for at least 2 to 4 weeks after the procedure. Scans performed before this time can reveal apparent fixed defects or are falsely positive for ischemia- these findings may be related to transient persistent myocyte dysfunction or spasm/endothelial damage at the site of the procedure. [31]
16. Papillary muscles
Insertions of the anterior and posterior papillary muscles may produce focal hot spots typically seen at the 2 (anterolateral) and 7 o'clock positions on short axis images. This finding may be misinterpreted as ischemia of other walls, particularly the inferior.
A corollary to this is the focal hot spots seen on the short axis images in the 7 and 11 o'clock positions in patients with significant right ventricular hypertrophy.
17. Diaphragmatic Creep
Patients with rapid and deep respiratory excursions following exercise are most likely to demonstrate a gradual upward shift in the position of the heart following exercise which produces an inferior/inferoseptal reversible defect. Waiting 5 -10 minutes prior to imaging generally eliminates this artifact. Cardiac creep is best appreciated on "column mode" sinogram images which register "cranocaudal" movement. The tomographic projection images for the column mode sinogram are summed and displayed as if you are facing the patient (coronal images). It is not appreciated on "row mode" sinogram images which register lateral movement. The tomographic projection images for the "row mode" sinogram are summed and displayed as if you were looking down from above the patient (transaxial images).
18. Patient Motion
Patient motion is a considerable problem in tomographic imaging which relies on a accurate center of rotation. Motion induced perfusion defects are affected by the type and amount of motion, motion timing, and the number of camera detectors [27]. Motion artifacts affect acquisitions with double-headed detectors more than acquisitions with a single-head detector. This assumption is related to the fact that a single occurrence of non-returning motion with a double-headed detector will affect twice as many projections as with a single-headed detector [27]. However, acquisitions with a single-headed detector are twice as long as with double-headed detectors for the same number of collected counts, and therefore, the chance that the patient will move during the acquisition is greater [27].With motion the heart develops a non-rounded, disjointed appearance.
Factors which affect the final result of motion include [27,28]:
1. Amount of movement: Less than 3mm is not usually visually detectable. Movement less than 6.5mm (1 pixel) is detectable, but is not usually clinically significant. Movement of 13mm or greater (2 pixels) frequently produces quantitative abnormalities. Motion correction programs can improve the exam, but studies with greater than 2 pixels of motion should be repeated [27].
2. Type of movement: Vertical movement (up and down) is usually more significant than lateral movement. Lateral motion, however, is more complex and will have a varying effect on the projection images [27]. For lateral motion, shifting is greatest in the anterior image (where motion is parallel to the detector) and least in the lateral image (where motion is perpendicular to the image) [27]. Patient bouncing usually does not produce significant perfusion abnormalities, whereas non-returning motion will create the largest defects [27].
3. Time of movement: Movement at the beginning or end of a study is less likely to result in image artifacts, whereas movement occurring at midaquisition has the worst effect- especially for double-headed detector systems [27]. As a general rule, motion in the projections in which myocardial counts are greater appears to cause larger motion artifacts [27].
4. Multiheaded camera: The second detector begins it acquisition at the point just beyond where the first detector completes its movement. Any movement which occurred during the exam will appear at this point in the rotating planar images.
18. Artifact
Remember- Perfusion defects occur in the distal tissues subtended by the stenotic artery. Defects involving the proximal septum and/or proximal anterior/anterolateral wall are unlikely to represent ischemia except in patients who have had CABG's. These patients may have high grade occlusions in their native proximal coronary arteries and hemodynamically significant stenoses in their saphenous vein or internal mammary artery grafts.
False Negative Thallium Exam
1. Beta blocker/Calcium channel blocker
Unable to obtain adequate stress
2. "Balanced" ischemia
Seen in symmetric 3 vessel disease
3. Insufficient luminal obstruction
4. Inadequate stress
5. Poor technique
Imaging is delayed following stress
REFERENCES:
(1) J Nucl Med 1993; Schulman DS, et al. Right ventricular thallium-201 kinetics in
pulmonary hypertension: relation to right ventricular size and function. 34: 1695-700
(2) New Engl J Med 1993; Zaret BL, Wackers FJ. Nuclear cardiology (1). 329: 775-783
(3) Am J Cardiol 1990; Villanueva FS, et al. Prevalence and correlates of increased lung/heart ratio of thallium-201 during dipyridamole stress imaging for suspected coronary artery disease. 66: 1324-28
(4) Am.J.Cardiol 1990; Lette J, et al. Transient left ventricular cavitary dilation during dipyridamole-thallium imaging as an indicator of severe coronary artery disease. 66:1163-70
(5) J Nucl Med 1994; Iskandrian AS, et al. When is myocardial viability an important clinical issue? 35 (Suppl): 4S-7S
(6) J Nucl Med 1994; Leavitt JI, et al. Demonstration of viable, stunned myocardium with technetium-99m-sestamibi. 35: 1805-07
(7) J Nucl Med 1992; Cuocolo A, et al. Identification of viable myocardium in patients with chronic coronary artery disease: comparison of thallium-201 scintigraphy with reinjection and technetium-99m-methoxyisobutyl isonitrile. 33: 505-511
(8) Circulation 1994; Dilsizian V, et al. Myocardial viability in patients with chronic coronary artery disease. Comparison of 99mTc-sestamibi with thallium reinjection and [18F] fluorodeoxyglucose. 89: 578-87
(9) Radiol Clin North Am 1993; Kiat H, et al. Myocardial perfusion imaging using technetium-99m radiopharmaceuticals. 31: 795-815
(10) J Nucl Med 1994; Altehoefer C, et al. Significance of defect severity in technetium-99m-MIBI SPECT at rest to assess myocardial viability: comparison with fluorine-18-FDG PET. 35: 569-74
(11) J Nucl Med 1995; Maurea S, et al. Enhanced detection of viable myocardium by technetium-99m-MIBI imaging after nitrate administration in chronic coronary artery disease. 36: 1945-52
(12) J Nucl Med 1995; Bisi G, et al. Technetium-99m-sestamibi imaging with nitrate infusion to detect viable hibernating myocardium and predict postrevascularization recovery. 36: 1994-2000
(13) J Nucl Med 1995; Maurea S, et al. Myocardial viability index in chronic coronary artery disease: technetium-99m-methoxy isobutyl isonitrile redistribution. 36: 1953-60
(14) Circulation 1994; 89:578-87
(15) J Nucl Med 1998; Bax JJ, et al. Comparison of Fluorine-18-FDG with rest-redistribution thallium SPECT to delineate viable myocardium and predict functional recovery after revascularization. 39: 1481-1486
(16) J Nucl Med 1995; Ohte N, et al. Clinical significance of reverse redistribution on
24-hour delayed imaging of exercise thallium-201 myocardial SPECT: comparison with
myocardial fluorine-18-FDG-PET imaging and left ventricular wall motion.
36: 86-92
(17) J Nucl Med 1993; Liu P, Burns RJ. Easy come, easy go: time to pause and put thallium reverse redistribution in perspective. 34: 1692-94
(18) J Nucl Med 1995; Soufer R, et al. Relationship between reverse redistribution on planar thallium scintigraphy and regional myocardial viability: a correlative PET study.36: 180-87
(19) Nucl Med Annual 1993; Parmett SR, Ongseng. Myocardial perfusion imaging: Pifalls and pearls. Ed. Freeman LM. Raven Press, NY. 195-221
(20) Radiographics 1999; Jadvar H, et al. SPECT and PET in the evaluation of coronary artery disease. 19: 915-926
(21) AJR 2000; Robinson VJB, et al. Causes of transient dilatation of the left ventricle during myocardial perfusion imaging. 174: 1349-1352
(22) Semin Nucl Med 1997; Kataoka T. False-positive myocardial perfusion scintigraphy in syndrome X. 27 (2): 186-189
(23) J Am Coll Cardiol 1996; Mazzanti M, et al. Identification of severe and extensive coronary artery disease by automatic measurement of transient ischemic dilatation of the left ventricle in dual-isotope myocardial perfusion SPECT. 27: 1612-1620
(24) J Nucl Med 2000; Verna E, at al. "False-positive" myocardial perfusion scintigraphy findings in patients with angiographically normal coronary arteries: Insights from intravascular sonography studies. 41: 1935-1940
(25) J Nucl Med 2001; Bax JJ, et al. Relationship between preoperative vaiability and postoperative improvement in LVEF and heart failure symptoms. 42: 79-86
(26) J Nucl Med 2001; Tawakol A, Gewirtz H. Does CABG improve left ventricular ejection fraction in patients with ischemic cardiomyopathy, and does it matter? 42: 87-90 (No abstract available)
(27) J Nucl Med 2001; Matsumoto N, et al. Quantitative assessment of motion artifacts and validation of a new motion correction program for myocardial perfusion SPECT. 42: 687-694
(28) J Nucl Med 1993; Nov.: p.1849
(29) J Am Coll Cardiol 1997 Bax JJ, et al. Accuracy of currently available techniques for prediction of functional recovery after revascularization in patients with left ventricular dysfunction due to chronic coronary artery disease: Pooled comparison data. 30: 1451-60
(30) Semin Nucl Med 2000; Bas JJ, et al. 18-Fluorodeoxyglucose imaging with positron emission tomography and single photon emission computed tomography: Cardiac applications. 30: 281-298
(31) Semin Nucl Med 1995; Newhouse HK, Wexler JP. Myocardial perfusion imaging for evaluating interventions in coronary artery disease. 25: 15-27
(32) J Nucl Med 2001; Tanaka R, Nakamura T. Time course evaluation of myocardial perfusion after reperfusion therapy by 99mTc-tetrofosmin SPECT in patients with acute myocardial infarction. 42: 1351-1358
(33) J Nucl Med 2001; Harel F, et al. Clinical impact of combination of scatter, attenuation correction, and depth-dependent resolution recovery for 201Tl studies. 42: 1451-56
(34) Radiology 2001; Oshinski JN, et al. Quantitative prediction of improvement in cardiac function after revascularization with MR imaging and modeling: Initial results. 221: 515-522