When it comes to screening of women with dense breasts, AI doesn't yield an improvement in performance over the combination of mammography and ultrasound without AI, according to research published July 26 in the American Journal of Roentgenology.
A team led by Si Eun Lee, MD, from Yonsei University in Yongin-si, South Korea, found that mammography with supplementary breast ultrasound had higher accuracy and specificity, as well as lower recall rate compared to mammography with AI and mammography with both ultrasound and AI.
"The findings fail to show a benefit of AI when performed in addition to supplementary ultrasound in patients with dense breasts undergoing screening mammography," Lee and co-authors wrote.
Standard mammography alone is not enough to definitively find breast cancer in women with dense breasts. For these women, supplementary imaging methods are used following mammography, with ultrasound being the most commonly used modality.
Previous research suggests that in the breast imaging setting, AI can aid radiologists in an adjunct role by helping with diagnosis. However, the researchers noted that results vary depending on the AI platform used.
For their current study, Lee and colleagues wanted to compare the performances of screening mammography, AI, and supplementary ultrasound by themselves as well as in combination with one another. It included retrospective data from 1,325 women with an average age of 53 years and who have dense breasts. The women underwent both mammography and ultrasound within a one-month interval in 2017. The team also used a commercially available AI tool (Insight version 1.1.0.0, Lunit) to assess the mammography exams.
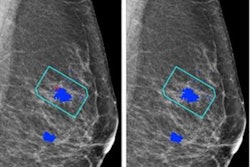
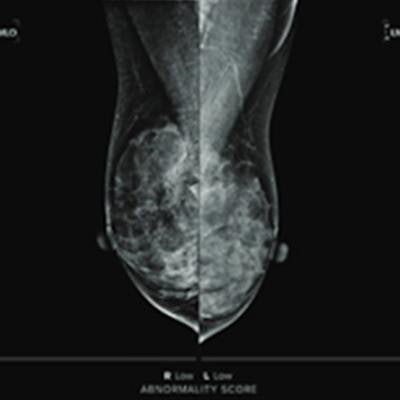
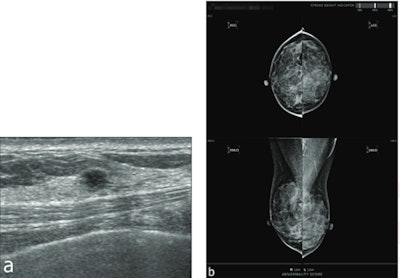 Images show results for a 57-year-old woman with dense breasts. Screening mammography (not shown) was assessed as BI-RADS category 2. (A) Supplementary screening breast ultrasound performed on same day as the mammogram shows a 4-mm round hypoechoic mass with angular margins in the right upper medial breast. (B) A screenshot shows the output of an AI tool, which assigned an abnormality score of "low" in each breast. Ultrasound-guided core biopsy and surgery showed an invasive ductal carcinoma, not otherwise specified (Luminal A, histologic grade I). This case represents a false-negative AI result. Image courtesy of ARRS.
Images show results for a 57-year-old woman with dense breasts. Screening mammography (not shown) was assessed as BI-RADS category 2. (A) Supplementary screening breast ultrasound performed on same day as the mammogram shows a 4-mm round hypoechoic mass with angular margins in the right upper medial breast. (B) A screenshot shows the output of an AI tool, which assigned an abnormality score of "low" in each breast. Ultrasound-guided core biopsy and surgery showed an invasive ductal carcinoma, not otherwise specified (Luminal A, histologic grade I). This case represents a false-negative AI result. Image courtesy of ARRS.The researchers reported that 12 cancers were diagnosed, including six invasive ductal carcinomas and six ductal carcinomas in situ (DCIS).
For standalone performance among the three methods, mammography demonstrated the highest accuracy (95.9%), specificity (96.2%), and sensitivity (96.2%). It also had the lowest recall rate at 4.4%. While AI had the highest cancer detection rate at 6.8 per 1,000 women, it also had the highest recall rate among the three methods at 11.9%.
When evaluating different combinations of the three methods, the researchers found that mammography with ultrasound outperformed other combinations.
| Performance comparisons for combinations of mammography, ultrasound, and AI | |||
| Mammography with AI and ultrasound | Mammography with AI | Mammography with ultrasound | |
| Cancer detection rate | 9.1 | 7.5 | 9.1 |
| Recall rate | 21.4 | 14.9 | 11.7 |
| Sensitivity | 100% | 83.3% | 100% |
| Specificity | 79.4% | 85.8% | 89.1% |
| Accuracy | 79.5% | 85.7% | 89.2% |
The researchers also reported that while ultrasound showed significantly improved measures over AI alone in women over the age of 50, these results were not significantly different in women under the age of 50. Additionally, mammography with AI and mammography with ultrasound showed no significant differences in recall rate, specificity, or accuracy in women under 50 years old.
The study authors wrote that this may be because younger women have denser breasts than older women, which usually changes the breast echotexture on ultrasound and adds to the challenge of interpreting breast images in these women.
However, AI did have its wins in the study. Although overall sensitivity between mammography and AI was not significantly different, AI detected one invasive ductal carcinoma and one DCIS that were missed on mammography. The researchers reported that one of these missed cancers was visible on mammography in a retrospective review.
AI, however, also missed three cancers, including one DCIS that showed grouped microcalcifications on mammography and two cancers deemed to be occult retrospective mammographic review but visible as masses on ultrasound.
The study authors suggested that based on their findings, the inclusion of AI is not an added benefit for breast cancer screening for women with dense breasts.
The full study can be found here.