By incorporating 3-tesla MRI, radiation oncology departments can look forward to a whole new world of bioanatomical information for guiding treatment planning, according to the chairman of the department of radiation oncology at Wake Forest University in Winston Salem, NC.
"Bioanatomic gross tumor volume (GTV) is actually much larger than the strict anatomic GTV, and that certainly has an impact on local control and survival," explained Dr. Edward Shaw during a talk at the Imaging Technologies for the Latest Radiation Therapy Treatment Planning symposium.
Shaw discussed the benefits of having a 3-tesla MR scanner in the radiation oncology suite at the symposium, which was sponsored by GE Healthcare of Chalfont St. Giles, U.K., and held concurrently with the 2007 American Society for Therapeutic Radiology and Oncology (ASTRO) meeting in Los Angeles.
Shaw told his audience that he relocated to Wake Forest University in 1995 as the department underwent a major physical overhaul. "We had the notion that, in our new department, we wanted the optimum anatomic imaging tools, and we recognized that the ability to image tumor biology and physiology was going to evolve over time," Shaw said.
The department's MR treatment planning room now houses a 3-tesla scanner and is staffed by an MR technologist, as well as two radiation therapy technologists who received additional training in MR.
"What's the difference between an MR scanner that you use for treatment planning and a diagnostic MR scanner that you have in radiology?" Shaw said. "The differences are that the patient is imaged directly in radiation treatment positioning with the opportunity to have the patient in the immobilization device. You would use a flat tabletop ... because obviously we treat on a flat tabletop. Then you have laser lights for referencing the patient for isocentric setup."
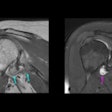
In terms of the actual imaging, Shaw emphasized that, for treatment planning, all MR images must be fused with CT. This anatomic data can then be used to calculate GTV, clinical tumor volume (CTV), and planning tumor volume (PTV), as well as visualize the normal structures.
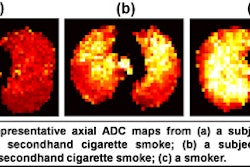
After that, it's pretty much anything goes as Shaw's group relies on a number of different MRI techniques for biological data: dynamic contrast-enhanced MR, diffusion tensor imaging (DTI), diffusion-weighted imaging (DWI), MR spectroscopy (MRS), and functional MRI (fMRI).
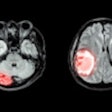
DTI for white matter tractography has been very helpful for assessing radiation-induced brain injury, according to Shaw. "The displacement of normal brain tissue, the pressure that that tissue may be under, may play an important role in the late effects of radiation (and) even acute effects like radiation necrosis. (DTI) is going to play an important role in normal tissue definition, particularly functional definition," he said.
MRS information has been invaluable in treatment planning for glioblastoma, Shaw noted. "(Glioblastoma) is a disease where there have been relatively few advances. We all treat these patients with 60 Gy over six weeks, and then when the patient enters follow-up, 95% of the time they emerge with local tumor recurrence. If you add spectroscopic data, you'll see that there are voxels surrounding the anatomic GTV that have a high concentration of tumor cells. If you add information from the dynamic contrast MRI, you'll see an area of increased perfusion, which represents increased tumor vascularity and burden," he said.
Finally, Shaw described fMRI as an "amazing technique" that allows clinicians to not only see the normal structures in action, but also develop information about the tolerance level of these structures during radiotherapy.
The ultimate value of 3-tesla MRI in the treatment planning room is that it gives radiation oncologists the ability to optimize control while minimizing the morbidity associated with radiation therapy, he said.
By Shalmali Pal
AuntMinnie.com staff writer
December 12, 2007
Related Reading
Glioblastoma survival rate quadrupled with temozolomide plus radiation, November 21, 2007
MR-guided intervention takes off in Japan, June 29, 2006
Copyright © 2007 AuntMinnie.com