"Rivers and seas boiling ... The dead rising from the grave ... Human sacrifice ... Cats and dogs living together, mass hysteria!" -- Ghostbusters, 1984
SAN ANTONIO - Implementing computed radiography (CR) and digital radiography (DR) systems in the same practice is not an apocalyptic event, although many administrators who have attempted to collocate the modalities would beg to differ. Radiology managers attending the American Healthcare Radiology Administrators (AHRA) annual meeting this week cited immense frustration in obtaining images of similar quality from the two modalities.
Based on the price of CR and DR systems, one might believe that the products would be engineered to work well directly out of the box. For the lucky few this assessment is correct, but the reality for most radiology professionals is that successful integration of the products into a practice will require multidisciplinary troubleshooting and implementation skills, according to David Piazzo.
"When we choose multiple vendors and multiple imaging systems, we may get multiple finished products out of the box," he said.
Piazzo, a radiologic technologist and application specialist in the CT injector division of Lake Success, NY-based E-Z-EM, shared his integration and implementation experience in a presentation on achieving CR and DR images of similar density and resolution from multiple acquisition sites.
The two devices use different methods of collecting x-ray energy: CR utilizes photostimulable storage phosphors, while DR systems generally use either flat-panel detectors or charge-coupled device technology. In addition, different vendors have diverse software applications to run the devices. This results in dissimilar DICOM header settings, hanging protocols, and window and level settings, according to Piazzo.
 |
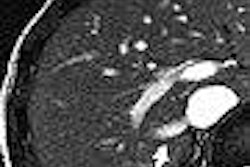
| The image above is from a CR system; the image below is from a DR system before standardizing the images. The pelvis phantom was imaged at a surface-to-image distance (SID) of 40 inches (100 cm), 80 kVp, and 50 mAs. Image courtesy of Larry Frederick and David Piazzo. |
 |
"If a chest x-ray done on one of your DRs looks similar to one done on your CRs, you do not have a major problem," he said. "If they don't, you will need to do some standardized testing."
A facility should start by having its x-ray tubes tested for output by a medical physicist. In particular, Piazzo advised, it will need to ensure that all the automatic exposure control (AEC) settings are very similar in output. He recommends that facilities use an anatomical phantom and a line-pair phantom for testing.
"Take identical exposures with the same phantom, at the same distance, in the same position, in the same position, and in the same heel/anode orientation, twice, for each x-ray modality," he said. "Once at a given kVp and mAs with the line-pair phantom, and once with the anatomical phantom at the AEC anatomical preset level that matches the phantom in use."
A side-by-side comparison will be needed. If the line-pair phantoms are dissimilar in density and resolution, either the output of the x-ray tubes is inconsistent, or one or more of the systems are not consistent with the others.
Piazzo recommends using a densitometer to measure density at the same three places -- a light, dark, and dense area -- on all the images. In addition, if multiple CR readers are being used by the practice, each reader will need to be tested with the line-pair phantom against the others through the same process.
Then the AEC images are compared. Piazzo suggested taking note of the rooms that produced variations when conducting the fixed kVp studies. The images should be compared for lightness and darkness, as well as contrast and graininess, and measured for density, according to Piazzo.
Once this information has been gathered, the facility will need to bring in the application engineers for each modality, the PACS applications engineers, and the medical physicist -- whose role is to act as the referee among the various groups.
The advantage of having all the relevant parties attending the same meeting is that one group cannot engage in blaming another group for the image quality problems; the testing information can be shared among all the parties simultaneously, and they can all work together to provide the practice with a homogenous image standard, he said.
"This will require that all the variables that the equipment has built into it are set to provide as homogenous an image as possible," Piazzo said. "Get your technologists to team with you on this project. Let them learn more about each system and see improvements as they happen. Let them share the pride in making the systems work better, enfranchising them into your solution."
To ensure consistent results from all the DR and CR devices in a practice, Piazzo strongly recommends using standardized protocols, both manual and AEC, for each imaging exam that are developed and set under the guidance of the radiologists and the assistance of the facility's technologists.
It is important to educate technologists that image density in CR and DR is not related to higher dose, at normal techniques, he added. However, a higher dose will result in a higher resolution. It is up to the practice to set standards on how much resolution is required for different studies, and to modify the manufacturer's recommended doses to fit its unique applications.
Piazzo also stressed that collimation is much more important with CR and DR than with film-based x-ray studies.
"If you're telling a CR or DR computer you are doing a chest, but you include everything from the jaw to the pelvis, it can only image average and not maximize the image processing algorithms you have set," he said.
Immediately after CR and DR protocols have been established, the department should perform quality assurance (QA) testing on the equipment and document all the variables in both hardware and software for each unit. This will provide a performance benchmark and allows the modalities to be recalibrated to optimal performance on an as-needed basis and as part of its regular QA program, Piazzo said.
By Jonathan S. Batchelor
AuntMinnie.com staff writer
August 11, 2005
Related Reading
Ortho group stumbles with DR, completes conversion to digital CR, May 27, 2005
New research shows CR more cost-effective than DR, February 28, 2005
Report finds vendors enable excess radiation doses in pediatric CR, DR, February 4, 2005
Study compares eight digital x-ray systems in clinical setting, December 24, 2004
DR looks good in CR, film comparison study, September 19, 2003
Copyright © 2005 AuntMinnie.com