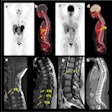
CHICAGO - A chest radiograph done in an emergency setting may provide a convenient opportunity to screen for vertebral fractures associated with osteoporosis, according to a multidisciplinary group from Canada. But the additional information doesn’t make it into the final radiology report often enough, according to Dr. Nancy Kim and colleagues at the University of Alberta in Edmonton.
“The prevalence of osteoporosis-related vertebral fractures (VF) in patients >60 years approaches 25%,” according to the 2003 RSNA poster presentation by the authors, who are from the departments of radiology, medicine, and emergency medicine at the tertiary care teaching hospital.
“[T]he presence of vertebral fracture mandates treatment, and by either improving routine reporting or using automated digital morphometry, we have an opportunity to improve the quality of osteoporosis care.”
The study population consisted of 100 randomly selected patients with a mean age of 75.2 years. Just over half of the patients were male. The majority of patients were eventually diagnosed with congestive heart failure (29%), cardiopulmonary disease (18% COPD), diabetes (18%), or other cardiac disease (18%). Twelve percent had a history of osteoporosis. However, the x-rays were selected without knowledge of the presenting complaints.
Two board-certified radiologists (a chest specialist and radiologist with experiences in osteoporosis clinical trials) independently reviewed the x-rays. The latter was considered the reference radiologist for this study. A resident trained in VF reading also read the exams. In addition, a validated and automated form of vertebral digital morphometry was undertaken. The lateral chest radiograph from T2-L2 was assessed.
“We defined a clinically important VF as one that was moderate-to-severe, i.e. a loss of height (greater than or equal to) 25% (wedge, crush, biconcave),” the authors explained.
According to the results, the prevalence of moderate-to-severe VF was 22% as assessed by the reference radiologist. The simple interobserver agreement was 87%-89% among reviewers, regardless of their experience level. The kappa values ranged from 0.56-0.58. The resident with VF training produced results that were equivalent to the radiologist. The greatest agreement (89%) was between the reference radiologist and digital morphometry (0.67 kappa).
Despite the prevalence of moderate-to-severe VF, only 12 of the 22 cases were mentioned in the official radiology report. In an interview with AuntMinnie.com, Kim attributed the underreporting to a lack of time and familiarity with VF amongst imaging specialists. But the fact that the resident in this study was just as adept at pinpointing VF as the more experienced radiologist indicates that a little training can go a long way.
“One of things that we learned with this study is that we can all confidently identify the presence of a fracture. I just think that VF is underappreciated,” Kim said. “We’re hoping with these kinds of studies that we’ll be able to develop a clinical pathway for treating these fractures.”
Checking for VF did not add any additional cost to the initial x-ray exam, she said. Kim’s team plans to update this research in the near future with a larger patient population (500) as well as information on the treatment outcomes for these patients.
By Shalmali Pal
AuntMinnie.com staff writer
December 1, 2003
Copyright © 2003 AuntMinnie.com