A survey of radiologists published in Radiology last year produced a shocking statistic: half of the doctors responding said they had been a defendant in a medical malpractice lawsuit.
Does this mean that half of our nation's radiologists are negligent? Not likely. Instead, the survey has a deeper meaning -- that the U.S. legal system is out of control and threatens to strangle sectors of healthcare that are critical to maintaining the welfare of our population.
One such sector is mammography. The U.S. is experiencing a medical liability crisis, which is fast getting away from radiologists, and mammography is headed toward being one of its casualties. Because of the threat of malpractice litigation, high liability insurance costs, and low reimbursement, radiologists are refusing to read mammograms, and radiology residents show no interest in specializing in breast imaging. This is occurring as demand for their services is rising due to an aging population.
This article outlines how the legal system has stacked the deck against mammography, creating a perfect storm of wily plaintiffs' attorneys, juries with unrealistic expectations, and mammography providers caught in the middle.
Mammography isn't perfect
Sickness and disease are in the cards for many of us, and death is inevitable. At times, though, our mortality can be hastened by the negligent actions of a physician, say by leaving a surgical instrument inside a patient, or cutting off the wrong limb. In such cases, no doubt exists in anyone's mind that the physician must be held accountable -- a legitimate medical malpractice case.
However, the norm in the U.S. is for lawyers to bait unsuspecting potential clients who may have suffered a health setback into becoming plaintiffs against anyone in the medical establishment who they believe could be responsible for their misfortune. What lawyers don't say, though, is that medicine is not an exact science. Instead, lawyers and the media have raised the public's expectation of medicine so high that physicians and healthcare practitioners are held to a perfect standard of care they cannot possibly attain.
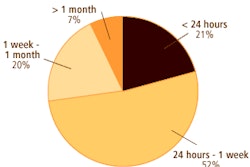
Along with ob/gyns and surgeons, radiologists are fast becoming the most popular targets for medical malpractice suits, with failure to diagnose breast cancer on mammography becoming an increasingly common accusation. How can that be, especially when mammography performed under the best conditions can have up to a 30% miss rate?
The answer is because malpractice litigation is an extremely lucrative undertaking, and breast cancer is a very emotional issue. Add together the wrenching picture of a young woman in her prime diagnosed with a fast-growing breast cancer, a lawyer who convinces her that the cancer should have been caught on a mammogram, a smooth-talking expert witness for the plaintiff, and a sympathetic jury, and you have a million-dollar verdict.
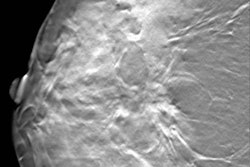
Though breast cancer has been around for thousands of years, mammography is fairly young. Through the years, breast imaging has matured from a simple clinical assessment into an all-inclusive evaluation. But mammography is still fallible -- miss rates are documented up to 30%.
But in court cases, the jury is not always told this fact. Or if it is, it is downplayed by the plaintiff's attorney. Breast cancer is not an easy disease to explain or diagnose, and reading a mammogram comes with its own innate difficulties. Breast cancer is not just one disease, but many, and the reasons for contracting it are varied.
For example, in a court case, a lay jury does not know that younger women have denser breasts in which cancer can grow faster, though their cancer risk is lower. As women age, their risk increases, their breasts are less dense, and the cancer tends to grow slower. As with anything else in medicine, though, this is not set in concrete. There are exceptions to rules. For instance, an older woman can have dense breasts with fast-growing breast cancer.
What else is a jury expected to understand? Microcalcifications, asymmetry, axillary tail of Spence, hindsight bias, lead-time bias, interval cancers, and dot size. Besides that, jurors have to listen to opposing expert witnesses telling them what the standard of care should be for that particular case.
In essence, we have a lay jury deciding whether a physician is guilty of medical malpractice -- if his or her actions have fallen below the standard of care -- all the while being expected to understand what it took the physician years to learn. In addition, you can have the same case tried in two different localities and have opposite verdicts. Lawyers thrive on this type of lawsuit.
A deterrent to negligence?
But are these lawsuits deterring legitimate negligence? Not nearly. After the case is tried, even if the verdict is for the plaintiff, there is no remediation for the "negligent" physician -- just an exchange of money. There is no understanding of why something happened.
Mammography does not cure or prevent breast cancer. Though it is the only tool we currently have available for detecting breast cancer at its earliest and most treatable stages, it has limitations. Why? Because it can't take into account the woman's history and the characteristics of her breast cancer, or the radiologist's experience and perception, image interpretation, and other factors.
Radiologists themselves will disagree on the interpretation of the same screening or diagnostic mammogram. Dr. Mark Klein of Washington, DC, says that it is documented that up to 67% of mammographically detected breast cancers missed on initial interpretation are visible in retrospect. However, this does not point to incompetence; it is a limitation of the technology.
So where do we go from here? Several tests for diagnosing breast cancer look promising. For example, MRI is currently being studied. However, it is not considered a screening test, but is used in conjunction with computer-aided detection (CAD). It also does not always distinguish correctly the difference between benign and cancerous conditions. PET can identify invasive ductal carcinoma, but can miss invasive lobular carcinoma. It also does not identify noninvasive tumors well.
It's a money thing. And, as in many arenas, education is the key. The public has to be informed, as well as educated. But unless we are personally involved as a plaintiff or a physician defendant, being human we don't usually care. Educating the public won't be an easy task.
Plaintiff trial lawyers vigorously defend the current legal status quo in the guise of protecting those who are "victims" of medical malpractice. It's pervasive. Go to www.classaction.com. You will see lawsuits involving the drugs Accutane, Bextra, Paxil, Vioxx, and Zyprexa, as well as Guidant and Medtronic defibrillators; the Logitech mouse; nursing homes; air, soil, and ground water contamination; body parts; and defective products. Nothing is sacred to plaintiff trial lawyers.
Tort reform is part of the answer, but trial attorneys have a powerful lobby against it, because the stakes are so high. In his recent State of the Union address, President Bush said doctors and nurses must be put back in charge of American medicine, instead of those in charge now -- bureaucrats, HMOs, and lawyers. He urged Congress to pass medical liability reform because a major cause of the high cost of healthcare is the threat of medical malpractice litigation to physicians. He's right, no matter what trial lawyers try to bamboozle the public into believing.
It's not just up to Congress, though. Every citizen has a duty to be a part of constructive political change. That is not always the case, though, because Americans tend to overlook serious matters unless an issue emerges up close and personal.
Many women are currently under the false impression that mammography is foolproof and that if the exam is done early enough and often enough, breast cancer can be detected, treated, and contained. This is misleading. However, change is inevitable, and technology is such that someday there will be a substitute for mammography.
Radiologists may disagree when, where, or how this will happen, but most agree that right now mammography is still the only tool available to diagnose breast cancer early enough to be treated, and we need to save it from extinction. To do this, the public must be educated as to not only the limitations of mammography, but that medicine is not a perfect science.
By René Jackson
AuntMinnie.com contributing writer
April 3, 2006
René Jackson is a registered nurse and the co-author of The Death of Mammography with Dr. Alberto Righi.
The opinions expressed in guest editorials are those of the author, and do not necessarily reflect the views of AuntMinnie.com.
Related Reading
Book review: The Death of Mammography, January 24, 2006
Sidestepping screening: What factors make women avoid annual mammography? October 10, 2005
Copyright © 2006 AuntMinnie.com