The Centers for Medicare and Medicaid Services (CMS) this week announced its final rule establishing a 3.3% increase in new payment rates for outpatient services starting January 1.
The increase, together with other policies contained in the final Outpatient Prospective Payment System (OPPS) rule, will increase projected Medicare payments to hospitals for outpatient services to $24.6 billion, compared to projected payments of $23.1 billion in 2004.
CMS is also significantly increasing payments for diagnostic mammograms by removing them from payment under the OPPS, as required by the Medicare Prescription Drug, Improvement and Modernization Act of 2003 (MMA). Like screening mammograms performed in hospital outpatient departments, diagnostic mammograms will be paid under the Medicare physician fee schedule, resulting in increases of nearly 40% over current OPPS rates for traditional mammograms, and about 60% for digital diagnostic mammograms.
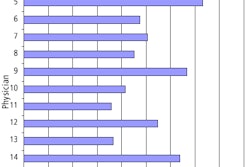
The rule also increases payment rates to hospitals for screening examinations that Medicare already covers. The final payment increases are as follows:
- Pelvic and breast exams to detect cervical and breast cancer, 1.7 %
- Barium enema to detect colorectal cancer, 2.1 %
- Bone density studies, 4.5 %
- Flexible sigmoidoscopy to detect colorectal cancer, 6.8 %
- Screening colonoscopy, also for colorectal cancer, 8.3 %
- Glaucoma screening, 9.9 %
In addition, the rule continues into 2005 the MMA provision that sets rates for brachytherapy sources on charges adjusted to cost, and establishes definitions for new codes for high-activity brachytherapy sources.
The final rule also responds to concerns raised during the comment period about proposed reductions in payments for procedures that require expensive devices. For 21 device-dependent ambulatory payment classification groups (APCs), the 2005 payment will be based on 95% of the 2004 payment median.
The rule will be published in the November 15 Federal Register. Comments will be accepted regarding new codes and their APC assignment during the 60-day period following publication. For more information, visit the CMS Web site at www.cms.hhs.gov.
By AuntMinnie.com staff writers
November 3, 2004
Related Reading
States, payors seek to stem tide of self-referral abuse, October 29, 2004
Making RVU-based productivity assessment work for you, October 29, 2004
CMS finalizes coverage for carotid artery stenting, October 13, 2004
Compliance program provides protection, metrics, August 2, 2004
Radiology group pays $2.5 million to settle alleged Medicare fraud, June 29, 2004
Copyright © 2004 AuntMinnie.com