Nuclear Imaging Tests
Radioactive Iodine Uptake Test (RAIU)
Technique
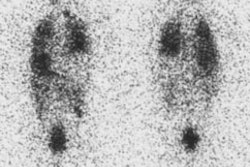
RAIU can be determined using either I-131 (7 uCi) or I-123 (200-300 uCi). Normal 24 hour RAIU is between 8 to 35%. Normal 4 hour RAIU is generally between 5 to 15%.
% Uptake= [(net neck counts - net thigh counts)x 100] /(net standard counts)
The RAIU test provides a useful assessment of thyroid function: in general, the higher the iodine uptake, the more active the gland. Note, however, that in patients with hypothyroidism such as Hashimoto's disease, the % uptake may be low, normal or high depending on the steps affected in thyroid hormone synthesis. This is therefore of no value in establishing the diagnosis of hypothyroidism.
RAIU test may be helpful in the following clinical conditions:
To confirm hyperthyroidism
To calculate therapeutic dose of I-131
To determine autonomous thyroid tissue (i.e. toxic nodules, - combined with thyroid scan)
To determine the cause of thyrotoxicosis*
* The most useful role of RAIU test is in determining the etiology of thyrotoxicosis. Thyrotoxicosis simply refers to excess thyroid hormone in the body and may be due to overactivity of the thyroid gland (hyperthyroidism), or other causes such as inflammation of the gland (thyroiditis) or ingestion of excess thyroid hormone. In "true hperthyroidism" - RAIU uptake will be high while thyrotoxic patients with thyroiditis or who abuse thyroid hormones will have a low RAIU. Other factors that affect RAIU uptake are listed below.
Factors affecting thyroid iodine uptake
Patient's iodine pool:
- Dietary variations: RAIU can be falsely elevated in patients who are iodine
deficient.
- Renal function: Poor renal function results in decreased excretion of iodine, the larger
iodine pool will compete with the radiopharmaceutical for uptake thus falsely lowering
RAIU.
- Recent iodine contrast study: The excess iodine will falsely lower the RAIU. It may
require weeks prior to scanning in order to obtain an accurate value. The Wolff-Chaikoff
effect refers to a transient decrease in iodide organification and hormone synthesis in
normal or Graves patients following an iodide load.
Medications
- Antithyroid drugs: Propythiouracil and methimazole result in a poor 24 hour scan because they block iodide oxidation and organification (and to a lesser extent thyroid hormone excretion). Because the agents do not inhibit iodine trapping, a pertechnetate scan, may be technically adequate.
- Thyroid hormone
- Amiodarone
Etiologies resulting in an Increased RAIU
* Hyperthyroidism (Grave's disease or TSH-secreting pituitary adenoma)
* Rebound following abrupt withdrawal of antithyroid meds
* Long term antithyroid therapy: Prolonged therapy may result in decreased circulating
levels of T4- hence TSH levels will increase. This will accentuate radioiodine uptake.
* Enzyme defects
* Iodine starvation
* Lithium Therapy
* Early Hashimoto's Thyroiditis (Patients rarely present at this stage, RAIU is typically
normal [early] or decreased [late] in these patients)
* Rebound during recovery from subacute thyroiditis
Etiologies resulting in a Decreased RAIU
* Blocked Trapping:
- Iodine load (most common). An iodine load can "falsely" lower the RAIU
through two mechanisms: 1) producing the Wolf-Chaikoff effect 2) causing a dilutional
effect, i.e., diluting the I-123 atoms with nonradioactive I-127 atoms.
- Exogenous thyroid hormone replacement depressing TSH levels
- Ectopic thyroid: Struma Ovarii
* Blocked Organification:
- Antithyroid medication (PTU): Note- Tc-99m uptake should not be affected
* Parenchymal Destruction:
- Acute, Subacute and Chronic Lymphocytic Thyroiditis
* Hypothyroidism:
- Primary or Secondary (insufficient pituitary TSH secretion)
- Surgical/Radioiodine Ablation of Thyroid
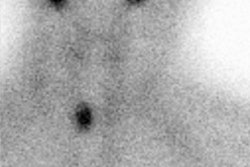
Thyroid Suppression Test
The thyroid suppression test is based on the premise that normal thyroid activity is suppressed by exogenously administered thyroid hormone. The test is used to determine the autonomy of a hot nodule or diffusely enlarged gland. A baseline scan and uptake are performed. The patient is then placed on T3 (Cytomel 25 ug TID [50-75 ug daily] for 7 days) to suppress TSH production. Iodine uptake should normally fall to 50% of presuppression value in a non-autonomously functioning nodule.
In most cases of hyperthyroidism, the diagnosis will be apparent on baseline scan and uptake. In Graves' disease, the uptake will be elevated with a homogenous distribution. In autonomous nodules, uptake may be high normal or elevated with the remainder of the normal gland suppressed. This together with the availability of sensitive TSH assays has virtually eliminated the need to do thyroid suppression test. Some conditions where this test may provide additional information include:
*Early Graves' disease with borderline hyperthyroidism or in euthyroid Graves' disease (patients presenting with opthalmopathy but normal function tests).
*Nodules which are indeterminate (warm or nondelinated) where a distinction between hot and cold is unclear. A repeat scan on cytommel (T3) or levothyroxine therapy with suppression of TSH may reveal whether the thyroid nodule is autonomous (hot on non autonomous (cold). A non autonomous nodule should be treated as a cold nodule and require further evaluation. [1]
*Evaluation of Toxic Multinodular Goiter (Plummer's Disease)
*Hypothyroid patients recently treated with I-131 for Graves' disease and started on hormone replacement may present with elevated thyroid hormone levels, suppressed TSH and show evidence of recurrent thyrotoxicosis. A high normal or elevated RAIU would confirm recurrent hyperthyroidism. However, a simpler alternative would be to discontinue hormone replacement and observe the patient.
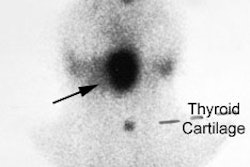
TSH Stimulation Test
The TSH stimulation test is used to identify thyroid tissue which is being suppressed by an autonomously functioning thyroid nodule (high levels of circulating thyroid hormone may suppress TSH release and thus, normal glandular function) or functioning thyroid metastasis.
Exogenous bovine TSH is administered once daily for 1 to 3 days. Suppressed normal thyroid tissue should be visualized following TSH stimulation. Patients with thyroid atrophy or diseased or damaged thyroid tissue will not have significant change in the appearance of their scans. Although this test was used frequently in the past to distinguish primary from secondary hypothyroidism, it no longer is necessary now that serum TSH levels are now available. In addition, the use of bovine protein may be associated with the risk of a major allergic reaction.
More recently, the administration of recombinant human TSH (rhTSH) has been proposed as an effective agent for detecting residual or metastatic thyroid tissue in patient with thyroid carcinoma. [MEIER CA et al. Diagnostic Use of Recombinant Human Thyrotropin in Patients with Thyroid Carcinoma, J Clin Endoc Metab 78:188-196, 1994] The traditional procedure for performing a follow-up whole body radioiodine scan requires the withdrawal of thyroid medications to allow endogenous TSH levels to increase above 40 mU/L so as to stimulate residual thyroid tissue. However, most patients become clinical hypothyroid during this period and are exposed to the potential risk of increased tumor growth associated with elevated serum TSH levels. Meier et al. reported in phase I/II study that the use of rhTSH was just as safe and effective in stimulating I-131 uptake by residual thyroid tissue without the disadvantages of having to withdraw thyroid hormones and causing hypothyroidism. Studies are still ongoing and currently, rhTSH is still not available for general clinical use.
Perchlorate Washout Test
This test is used to identify congenital or acquired organification defects which most commonly involves the enzyme iodide peroxidase. In normal subjects, radioiodine when taken up by the thyroid is immediately organified and bound to thyroglobulin. However, in patients with defects in peroxidase activity (usually hypothyoid), trapped radioiodine is rapidly discharged when sodium perchlorate (an inhibitor of thyroid iodide trapping) is administered.
Thyroid uptake is then determined between 2 and 4 hours after administration of the dose. Potassium perchlorate 109 mg/kg is then administered orally and a repeat measurement of RAIU performed in 30 to 60 minutes. A decrease in RAIU greater than 10-15% following perchlorate administration is indicative of any organification defect. The test is rarely performed since the treatment for primary hypothyroidism is thyroid hormone replacement regardless of the cause or site of defective thyroid hormone synthesis.
Thyroid Scintigraphy and Pregnancy:
Pregnancy is an absolute contraindication to thyroid scanning, especially after the 12th week of gestation when the fetal thyroid begins to trap iodine. Prior to this time tests should be avoided if possible despite the fact that the fetal dose will be very low (1 mrad/mCi of I-131). Iodine, Thionamides, Thyroid Stimulating Antibodies, and TRH all cross the placenta easily. T3 and T4 cross only minimally. TSH does not cross the placenta.
REFERENCES:
(1) J Clin Endoc Metab 1992; Ridgway et.al. Clinical Review 30: Clinician's Evaluation
of a Solitary Thyroid Nodule. 74: 231-235