Thyroid Physiology and Function Testing
TRH/TSH
Thyroid Releasing Hormone (TRH) is a peptide hormone synthesized in the hypothalamus and passed through the hypophyseal portal venous system. In the anterior pituitary, TRH stimulates synthesis and release of Thyrotropin (TSH). TSH in turn acts on the thyroid glad to stimulate thyroid gland growth and thyroid hormone synthesis. A simple negative feedback relationship exists between the pituitary and the thyroid. The release of TSH is inhibited at the pituitary by elevated circulating levels of thyroxine (T4) that is converted by intrapituitary type II deiodinase to triidothyronine (T3).
Thyroid Hormone Synthesis
There are 4 basic steps involved in thyroid hormone synthesis which include:
- Iodide trapping - iodide is actively transported into the thyroid gland
- Organification - the enzyme thyroid peroxidase using tyrosine and iodide as substrates, forms inactive iodotyrosines: 3--monoiodotyrosine (MIT) and 3,5-Diidotyrosine (DIT). The tyrosine residues MIT and DIT are incorporated into the soluble protein thyroglobulin which is stored as colloid in the follicular lumen.
- Coupling - the enzyme thyroid peroxidase catalyzed the coupling of MIT + DIT to form triidothyronine (T3) and the coupling of DIT + DIT to form thyroxine (T4).
- Proteolysis or release - proteolysis of thyroglobulin produces the active hormones T4 and T3, which are then secreted into the blood.
Approximately 90% of the released thyroid hormone is in the form of T4, and 10% in the form of T3. The great majority of T3 (80-90%) is produced by the peripheral conversion of T4. The metabolic activity of thyroid hormone is determined by the amount of free T3 and free T4. Thyroxine (T4) is very highly protein bound to thyroid binding globulin in plasma (99.95% bound, about 0.05% free). Therefore, a rough estimate of the total T4 can be approximated by the amount of bound thyroxine.
Tri-iodothyronine (T3) is produced by the peripheral deiodination of T4. T3 is much more potent than T4. About 99.5% of circulating T3 is bound (0.5% free). Reverse T3 is also produced by the deiodination of T4, but only when there is excess circulating thyroid hormone (hyperthyroid states). Reverse T3 is not physiologically active, so its production helps to prevent excess catabolism. Levels of reverse T3 are also elevated during periods of severe illness. Elevated levels of reverse T3 are also present during periods of severe nonthyroidal illness such as sepsis, congestive heart failure or burns. Since reverse T3 is not physiologically active, the conversion of T4 to T3 instead of the more active T3 is a metabolic compensation to prevent excess catabolism.
Thyroid Hormone Transport/TBG
More than 99% of thyroid hormone is carried in circulation firmly bound to three major binding proteins: thyroid binding globulin (TBG), transthyretin (TTR, formerly called thyroxine binding pre-albumin - TBPA) and albumin. TBG is the primary serum binding protein because of its higher affinity for T4. Under normal conditions, 75% of T4 is bound to TBG, 10-15% to TTR, and 5-15% to albumin. When bound, T4 is not physiologically active but provides a storage pool of thyroid hormone which can last 2-3 months (mean half-life of T4=6.7 days in adults).
TBG is synthesized by the liver under the influence of estrogen. An increase in TBG concentration in response to higher estrogen levels may result in higher measured total T4 concentration. However, the amount of free T4 concentration remains constant and the patient remains clinically euthyroid.
Conditions associated with increased levels of TBG:
- Estrogen Effects - pregnancy, oral contraceptives
- Infectious Hepatitis
- Biliary Cirrhosis
- Genetic Determination
In contrast, factors that cause a decrease in TBG concentration or lower affinity for T4 binding to TBG may result in low measured total T4 concentration without affecting free T4 levels.
Conditions associated with decreased binding of T4 by TBG:
- Androgens and Anabolic Steroids
- Large doses of Glucocorticoids
- Nephrotic Syndrome
- Major Systemic Nonthyroidal Illness
- Active Acromegaly
- Chronic Liver Disease
- Drugs - dilantin, tegretol
- Genetic Determination
Thyroid Function Tests
Total serum thyroxine (T4)
This includes both bound and free T4 concentration. Under most conditions with normal TBG concentrations, the total T4 level reflects the functional state of the thyroid. However, changes in binding proteins as described above, may alter total T4 concentration without affecting the unbound free T4 level. In these circumstances, calculating the free thyroxine index (FT4I) or obtaining a direct free T4 or free T3 level would provide a more accurate estimate of the patients true thyroid status.
T3 resin uptake (T3RU)
This test has been renamed thyroid hormone binding index (THBI) or thyroid hormone binding ratio (THBR), although most clinicians are still more familiar with the use of the term T3RU. It is important not to confuse T3RU with the serum total T3 by radioimmunoassay (total T3-RIA) that measures the total serum triidothyronine (T3) concentration. The T3 Resin uptake test measures the amount of unsaturated binding sites on the thyroid hormone transport proteins. A proportion of the labeled T3 will bind to available sites on the serum TBG; any excess will bind to the resin. Resin uptake is inversely proportional to the number of vacant binding sites, and therefore inversely proportional to the total TBG.
In thyrotoxicosis, there are fewer vacant binding sites available on thyroxine binding globulin due to the high circulating levels of thyroid hormone. This means less radioactive T3 will be able to bind to TBG and more will bind to the resin. Hence, resin uptake is higher in hyperthyroid patients than it is in normals. The converse is true in hypothyroid states. In high TBG states, such as pregnancy or estrogen therapy, the T3RU will be low. However the physiologically active free thyroxine level will still be normal.
Free thyroxine Index (FT4I)
FT4I is a reflection of the amount of free hormone (free T4) in most situations. It is a calculated value and corrects for changes in TBG concentrations by using the following formula:
FTI = (Total T4) X (T3 Resin Uptake / T 3RU control).
Mean normal T3RU for the particular assay (i.e. normal range 25-35% mean normal is 30%)
With extreme changes in TBG concentrations, acute medical illness, heparin therapy or low protein states secondary to nephrotic syndrome, the FT4I may not accurately reflect the amount of free T4 concentrations.
Free T4 and T3
More direct methods are now available for measuring free T4 and T3 levels. These tests have replaced the FT4I and FT3I in many centers. In reality, most methods of measuring "free T4" provide only indirect estimates of true levels of circulating free hormone and its accuracy may be affected by severe TBG changes or alterations in binding protein affinity. The gold standard for obtaining a true free T4 concentration is by direct equilibrium dialysis but is limited by cost and availability.
TSH
The development of new sensitive immunoradiometric (IRMA) assays to measure serum thyroid hormone (TSH, thyrotropin) has been a valuable tool in the diagnosis and management of thyroid diseases. The expected normal range for TSH is 0.5-5.0 mU/L. Older insensitive TSH-RIA assays could only measure concentrations as low as 0.5 mU/L. With the new sensitive TSH assays, TSH concentrations as low as 0.001 mU/L can be detected.
Measuring the serum TSH has become the screen test of choice for thyroid disease. Primary hypothyroidism produces elevated TSH levels whereas patients with primary hyperthyroidism (i.e. Graves) should have undetectable TSH values. This relationship is true only in individuals with an intact hypothalamic-pituitary-thyroid axis. Patients who present with a normal or detectable TSH level and elevated thyroid hormone concentrations require further evaluation to exclude central causes of hyperthyroidism.
TRH test
The administration of thyrotropin releasing hormone (TRH) causes a rise in TSH concentration in normal subjects (TSH = 2-30 MU/L.) An exaggerated response occurs in primary hypothyroid subjects (TSH often > 30 mU/L, depending on the baseline TSH elevation.) Hyperthyroid patients have a mild or absent TSH response (TSH < 2 m U/L) since the suppressed TSH cannot be stimulated by exogenous TRH. The introduction of sensitive TSH assays that can detect low suppressed TSH levels, identifying patients with primary hyperthyroidism, has virtually made the TRH stimulation test obsolete.
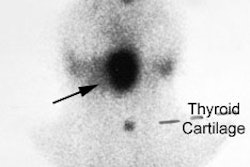
Iodine
Plasma iodine in the form of iodide is concentrated (trapped) in the thyroid cells by an energy requiring active transport mechanism where it is incorporated into T3 (triiodothyronine) and T4 (thyroxine) via organification (Therefore, iodine measures both trapping and organification by the thyroid gland). These active hormones are stored in follicles as thyroglobulin.
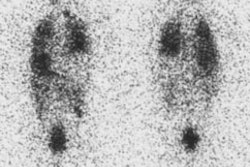
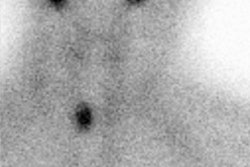
The normal distribution of iodine, and therefore its radiotracer isotopes, is in the thyroid, salivary glands, gastric mucosa, small and large bowel, urinary bladder, liver, and breast (esp. during lactation; see below). Iodine undergoes both renal (up to 75% in 24 hours) and GI excretion.
The normal daily dietary intake of iodine is about 500 ug. The amount of iodine in a typical uptake dose (10 uCi) is about 8 nanograms. This is significantly less than the amount of iodine in I.V. contrast- which, assuming a 40% content of iodine, contains about 40 grams of iodine in 100 ml.
Iodine Deficiency Goiter
Iodine deficiency goiters are the result of chronic TSH stimulation. Patients have elevated TSH levels and low serum T4 (due to lack of iodine for hormone synthesis). RAIU is increased due to the glands need for iodine.
Fetal and Neonatal Thyroid Function
Iodine and technetium both cross the placenta and will be concentrated in the fetal thyroid. The fetal thyroid does not concentrate iodine during the first 12 weeks of gestation; beyond this point, iodine uptake increases progressively until term. There is probably only minimal transfer of maternal TSH, T4 and T3 across the placenta. However, Iodine, Thionamides, and TRH can cross the placenta without difficulty. The fetal thyroid is highly sensitive to acute iodine overload [2]. Elevated levels of plasma iodine inhibbit biosynthesis and secretion of thyroid hormones (this is an autoregulatory process known as the Wolff-Chaikoff effect) [2]. The fetal thyroid may not be able to escape from the transient inhibitory effect of excess iodine until approximately 36-40 weeks of gestation [2]. Susceptability to fetal hypothyroidism is greatest between 18-36 weeks gestation [2]. However, a review of a small number of patients that had received iodinated contrast during pregnancy found no ill effect on neonatal thyroid function [2].
Following delivery there is an abrupt increase in serum TSH and thyroid uptake of iodine is elevated from 10 hours to 2 days post-delivery. TSH levels and uptake return to normal levels within a few days. Both Iodine and Technetium are secreted in the breast milk of lactating women, so nursing should be delayed for 48-72 hours following Tc99m, and for 2-3 weeks following I-131 imaging- essentially this translates to discontinuance of breast feeding. We recommend that women who are breast feeding permanently discontinue breast feeding if they are to undergo I-131 therapy.
REFERENCES:
(1) Radiographics 2003; Intenzo CM, et al. Scintigraphic manifestations of thyrotoxicosis. 23: 857-869
(2) AJR 2008; Atwell TD, et al. Neonatal thyroid function after
administration of IV iodinated contrast agent to 21 pregnant patients. 191:
268-271