Radionuclides
Iodine-123
I-123 decays by electron capture, has a physical half-life of 13.6 hours, and a gamma energy of 159 keV. It is produced in a cyclotron by either one of two methods:
I-127(p,5n) Xe 123 -> I 123
This method requires more energy, but produces I-123 of higher purity with no I-124 contamination and very little I-125 (I-125 has a half-life 60 days and emits 25 to 35 keV x-rays which contribute significantly to the radiation exposure to the patient). Because I-123 decays much faster than these contaminants, doses which are more than 24 hours old should not be used.
Te-124 (p,2n) I-123
This method results in impurities such as I-124 (5%), I-125, I-126, and Na-24. The I-124 has higher energy gamma emissions and a 4.2 day half-life which contribute to image degradation and patient dose, respectively.
Dose
200-400 uCi
Distribution:
Iodine is concentrated normally in the thyroid, choroid plexus, salivary glands, nasophaynx, stomach, bowel, mammary glands in females, urinary tract and bladder (secondary to excretion), and occasionally in the nasal mucosa [2].
Indications
The use of I-123 for thyroid imaging permits evaluation of the entire metabolic iodine pathway including trapping, organification, coupling, hormone storage, and secretion [1]. I-123 is the agent of choice when evaluating substernal goiters because there is usually substantial mediastinal blood pool activity associated with Tc-pertechnetate. The maximal count rate in the thyroid occurs approximately 6 hours following the oral administration of the agent. Images are typically acquired 4 hours following administration of the tracer, and uptake values are determined at 4 and 24 hours. The uptake of radioiodine by the follicular trapping system is decreased by perchlorate, thiocyanate ions, and expansion of the circulating iodine pool from dietary and medical sources (IV contrast, amiodarone) [1]. Antithyroid drugs (such as propylthiouracil and methimazole) will interfere with organification, coupling, and tracer storage in the thyroid gland and the 24 hour scan will be suboptimal [1,2]. Because these agents do not inhibit iodine trapping, a scan made several hours after dose administration may be technically adequate [2].
Contraindications
Pregnancy is an absolute contraindication to I-123 thyroid scanning after the 12th week of gestation when the fetal thyroid begins to trap iodine [2]. Breast feeding is a relative contraindication to thyroid scanning because about 20% of an administered dose is excreted in breast milk [2].
Iodine-131
Iodine-125
I-125 is not used for imaging. The agent decays by electron capture with a physical half-life of 60.2 days. It emits a gamma photon of 35 keV. The agent is primarily used for radioimmunoassays and other in vitro procedures.
Technetium-99m Pertechnetate
- Patient has been taking thyroid blocking agents (Propylthiouracil). Thiouracil blocks oxidation and organification of iodide following its uptake by the thyroid gland, but will not interfere with trapping of pertechnetate.
- Patient is unable to take medication orally
- The study must be completed in < 2 hrs
- Thyroid function (uptake studies) are not necessary
Pertechnetate (TcO4-) is a monovalent anion trapped by the thyroid gland in the same manner as iodine (an active transport mechanism). After trapping pertechnetate slowly "washes" from the gland- it does NOT undergo organification. Peak thyroid activity occurs between 20 and 40 minutes after injection. Only 2-4% of the administered dose is trapped in the thyroid. Pertechnetate is secreted in human milk (discontinue breast feeding for 48 hours after dosing) and also crosses the placenta to accumulate in the fetus.
Iodine and pertechnetate share the same active transport uptake pathway. The uptake pertecnetate by the follicular trapping system is decreased by perchlorate, thiocyanate ions, and expansion of the circulating iodide pool (iodinated contrast, dietary, or the antiarrhythmic agent amiodarone). Pertecnetate uptake should not be significantly affected by PTU or Tapozole which interfere with organification.
The typical dose used for thyroid imaging is 3 to 10 mCi intravenously.
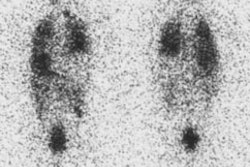
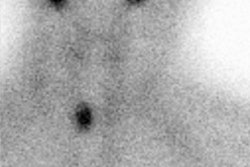
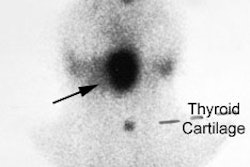
Imaging is performed approximately 15 to 20 minutes after tracer administration. Anterior and oblique images are acquired using a pinhole collimator with a 3.5 mm aperture (100,000 counts each image) [3]. An anterior planar image from the sternal notch to the salivary glands is also obtained. This image should be performed with a length marker so that the size of the gland can be assessed. Iodine uptake is calculated using a small dose of I-131 (5 uCi) [3]. Dr. Fink-Bennet feels that a rough estimate of thyroid uptake can be obtained from the Tc-pertechnetate exam by obtaining a 1 minute anterior planar image over the thyroid and salivary glands 5 minutes after injection of the tracer. A hypofunctioning gland will appear less intense than the salivary glands, a normal gland equal to the salivary glands, and a hyperfunctioning thyroid hotter than the salivary glands.
When using Tc-99m for thyroid imaging, scans can be completed in a much shorter time due to the larger dose [3]. However, in comparison to I-123 studies, more background activity is usually present on pertechnetate images. Linear esophageal activity, due to tracer secreted by the salivary glands which is swallowed, may be seen. This can be cleared from the esophagus by drinking water. (Note: See Pyramidal Lobe below). A pinhole collimator is used for enhanced resolution and also facilitates oblique views.
The size of nodules that can be detected by pertechnetate imaging depends upon the nodules function and size. Hot nodules may be seen even if they are very small, but a hypofunctioning nodule less than 0.8 to 1.0 cm in size lying within the gland may not be discernible [1]. In general, Tc-pertechnetate 5-mm pinhole imaging has a sensitivity of 80 to 95% for cold nodules between 8 to 18 mm, but nearly 0% for nodules less than 5 mm.
There are reported cases of thyroid carcinomas that are capable of trapping, but not organifying iodine (a "discordant" nodule which will appear warm or hot on pertechnetate imaging, but cold on the I-123 scan). About 5% of thyroid cancers can manifest as discordant nodules [3]. Therefore, any patient with a non-cold nodule on a Tc-99m scan should be repeated with I-123 to avoid this disparity. Cold nodules with Tc-99m scan will inevitably be cold with an I-123 scan.
The uptake of Tc-99m-pertechnetate by the follicular trapping system is decreased by perchlorate and expansion of the circulating iodine pool from dietary and medical sources (IV contrast, amiodarone) [1]. Antithyroid drugs do not inhibit iodine trapping and therefore pertechnetate can be used when imaging these patients [2].
At least 48 hours should elapse after a pertechnetate scan before resuming breast feeding [2].
Pertechnetate is the preferred imaging agent when:
Radiation dose to the thyroid, by agent
Assuming normal sized adult gland (20 gm) with normal RAIU (15%):
* I-131: 800-1000 rad/mCi; 16,000 rad/mCi in the neonate
* I-123: 7.5 rad/mCi (adult); 160 rad/mCi (neonate)
* I-125: 450 rad/mCi
* 99mTc-O4: 0.13 rad/mCi (adult); 3.4 rad/mCi (neonate)
REFERENCES:
1. Endocrinology and Metabolism Clinics of North America 1990; Shulkin BL, Shapiro B. The role of imaging tests in the diagnosis of thyroid carcinoma. 19: 523-541
2. Thyroid and whole-body imaging. Charkes ND. In The Thyroid, 5th ed. Ed Ingbar and Braverman. Lippincott, Philadelphia, 1986. 458-478
3. Radiographics 2003; Intenzo CM, et al. Scintigraphic manifestations of thyrotoxicosis. 23: 857-869
4. J Nucl Med 2005; Robbins RJ, et al. The evolving role of 131I for the treatment of differentiated thyroid carcinoma. 46: 28S-37S