The raw numbers aren't encouraging. According to a recent Society of Pediatric Radiology report, 100 pediatric radiology positions went unfilled in the U.S. in 2003; by the end of 2004 the total had risen to 117.
A protracted shortage of pediatric subspecialists is leading to children's imaging studies being read by radiologists without special training -- who may not be particularly comfortable doing so. And the pediatric imaging case load continues to rise by 4% to 6% per year.
Can this subspecialty be saved? Is it even in crisis? Dr. Robert T. Bramson and Dr. George A. Taylor from Children's Hospital Boston and Harvard Medical School seem to think so. In a June Radiology editorial, the authors warned that if radiology is unable to meet the demand for pediatric radiologists, "pediatric radiology could quickly reach its tipping point. In the best of the bad-case scenarios, the marketplace will force adult radiologists to perform pediatric radiology studies. In the worst-case scenarios, the various pediatric clinical specialists will fill the vacuum and perform the pediatric imaging" (Radiology, June 2005, 2005, Vol. 235, pp. 719-722).
Making no claims of originality, the authors suggested a number of creative ideas for reinventing pediatric radiology, including making pediatric radiology attractive to increase the number of recruits, and reducing barriers to entry in the field. AuntMinnie.com also spoke with a couple of pediatric radiologists who had suggestions of their own.
The Radiology authors ticked off several trends they believe are conspiring to suppress the pediatric radiologist head count. First, they noted, pediatric radiologists represent the single oldest subspecialty in practice -- up to 10 years older on average than the runners-up, oncologists. Even if no one were to retire, it would take three to five years just to fill the existing available positions, they stated. And fewer applicants seem to be vying for fellowship positions.
"On the basis of our own experience and what we have learned from others, the number of applicants for pediatric radiology fellowship positions either remains stable or, in recent years, has had several periods of decline," the authors wrote. "No new fellowship training programs are being added, and many existing programs risk losing their accreditation because they have had no trainees in several years."
Meanwhile, most radiology groups are seeing their annual workload increase by 4% to 6%, with growth as high as 5% to 6% in pediatric radiology. The trend is similar in pediatric hospitals, as measured in relative value units (RVUs), the team wrote.
But lest any of this sound like a lucrative deal for the remaining pediatric radiologists, the authors are quick to note that high demand for interpretation of children's imaging studies doesn't appear to be driving up salaries. For one thing, third-party payors are getting ever more tightfisted, the authors note, and thereby are exerting a significant downward force on the economics of the subspecialty.
In increasingly sophisticated efforts to control costs, payors are instituting complex preauthorization requirements, refusing to authorize more complex imaging exams they are calling medically unnecessary, and diverting more expensive imaging studies, including CT and MRI exams, away from academic centers and toward less expensive providers, Bramson and Taylor wrote.
"At our pediatric institution we interpret or provide a second opinion on CT or MR images obtained outside our institution approximately 3,000 times each year," they wrote. "The studies are performed at other locations either because third-party payors referred them there, as a part of a program like National Imaging Associates, or because a pediatric radiologist was not available at that location to obtain and interpret the images."
Accompanying these trends are self-referral pressures that are exacting their own toll on the subspecialty. Today there are nephrologists and urologists who want to perform their own renal ultrasound (US) studies, orthopedic surgeons who want to interpret their own musculoskeletal MR images, and emergency room physicians advocating their own use of US for abdominal trauma, the researchers wrote, noting that radiology does not have a good track record of holding onto specialized turf.
These trends contribute to the current situation of pediatric radiologists, who must often do extra work with little or no financial compensation, they concluded. The authors recommended several steps for improving the prospects of the subspecialty.
Increase the number of pediatric radiologists
"Radiology must demonstrate that pediatric radiology is an exciting, attractive career choice for young physicians in training -- the earlier in their training they get this message, the better," the authors wrote. "Pediatric radiologists need to aggressively move into the lecture circuit for medical students and radiology residents. They should participate in the development of a national medical student curriculum in radiology."
Frequent exposure to pediatric radiology helps keeps the subspecialty on the minds of potential recruits, enabling them to see the effect pediatric radiologists can have on children's lives, the authors wrote. Such exposure is increasingly important in a workplace culture that is undergoing a sea change in traditional notions of loyalty and job satisfaction.
"When a company or organization crosses a certain threshold and its market share drops below a certain percentage, it loses its relevance, and the marketplace looks for alternative solutions to the problems that the organization was solving," Bramson and Taylor wrote. In order to survive, pediatric radiology must reinvent itself, and it can, provided that its leaders recognize the impending crisis and take action to preserve the subspecialty, the group wrote. One way of reshaping the subspecialty is examining and perhaps reshuffling the associated job duties.
"Radiology needs to take a serious look at the ways in which pediatric radiologists add value to the diagnostic process," Bramson and Taylor wrote. "Does it really take someone with full residencies in pediatrics and radiology, a two-year fellowship in pediatric radiology, and 20 years of clinical experience to interpret follow-up fracture images or the fifth scoliosis series? If we add no meaningful value to the care of the child, then let's not do it, or let's delegate the activity to a more appropriate level of training or expertise."
Reduce entry barriers
The pathways to certification need to be examined, recreated, and streamlined where necessary, the authors opined. The development of a focused "pediatric track" during radiology residency is one suggestion that may have merit.
"The American Board of Radiology has approved an experimental pathway called Pediatric Emphasis Diagnostic Radiology Alternative Pathway, or PEDRAP," Bramson and Taylor wrote. "With this plan, radiology residents would spend half of their time during residency training focused on pediatric radiology and the other half focused on adult radiology. The radiology resident who follows this training pathway will likely have come from a background in pediatrics.... Some leaders have suggested a variation on the procedure, such as identifying pediatricians interested in radiology and building a special training program for them."
Board certification and other issues would need to be resolved, but eliminating the fellowship year could make radiology more attractive to pediatricians who are interested in imaging but wary of the lengthy training path.
It is unclear how the problem of board certification with special qualification in pediatric radiology will be handled with either of these two suggestions, but the issues do need to be resolved, the team noted. If the fellowship year could be eliminated, the field might see itself becoming more attractive to some pediatricians who might prefer practicing radiology to pediatrics but abhor the training requirements.
Expand the pediatric radiology workforce and increase efficiency
If pediatric radiologists are overspecialized, redistributing the workload and the tasks may produce more efficient workflow patterns, they authors suggested.
Technologists might welcome an expanded career pathway, for example. With formal training, the model practice could include a specific list of expanded tasks, especially the more routine ones, that this group could perform under the supervision of radiologists, the team wrote.
"The American College of Radiology is currently discussing these possibilities," Bramson and Taylor noted. "Perhaps pediatric radiology is the right environment and gives us the opportunity to test this experiment.... Other specialties have used physician extenders or physician assistants. Why not radiology?"
Another suggestion lauds the use of PACS networks, enabling subspecialists like pediatric radiologists to extend their expertise "beyond the geographic borders of their institutions," the team wrote. "This could, in theory, supply needed services to some remote locations or to those without a pediatric radiologist available. Clearly, this will only help with the misdistribution of pediatric radiologists. There still needs to be a sufficient number of pediatric radiologists available to actually perform the work."
In today's practice environment, efficiency often takes a back seat to competitive concerns, they noted. Thus, several groups in a geographic area might have a pediatric radiologist who, lacking enough young patients to fill the day, spends much of the workday reading adult studies. The authors hope that a method could be devised for sharing the interpretation of such images among practices without fears of lost revenue or lost business opportunities.
Macroeconomics
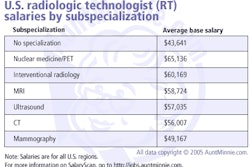
Myriad other economic realities conspire to keep pediatric radiology lower-paid than adult specialties, Bramson and Taylor wrote. For example, pediatric radiologists perform fewer high-tech imaging exams such as CT and MR procedures. Moreover, it generally takes longer to acquire and read children's images, leading to lower imaging volume and lower compensation.
"Radiology needs to make a convincing case to third-party payors that a premium should be paid for subspecialty work done by pediatric radiologists," Bramson and Taylor wrote. "This may require a joint educational effort to persuade parents that a study performed by a pediatric radiologist is more likely to satisfy the needs and consider the peculiar demands of children and their parents, intuitively resulting in a better study for the child."
"Leaders need to acknowledge that a problem exists and take bold innovative steps," they concluded. "We need to try different, unique, and innovative methods…. An organization will not adapt unless someone steps up and provides some direction that the organization can take. Who is going to provide that leadership? Can we save pediatric radiology? Do we want to expend the energy, try the experiments, suffer the failures, and find a way to avoid the tipping point that spells the demise of pediatric radiology?"
Other ideas
"I believe that providing adequate support for practicing radiologists is key," wrote Dr. Mark Halsted, a pediatric radiologist and chief of informatics research at Cincinnati Children's Hospital in Ohio. "Hiring a robust ancillary support staff, implementing helpful informatics resources, and hiring resources such as a pediatrician to perform patient sedations, thereby freeing pediatric radiologists to interpret studies, are all helpful measures that we have successfully implemented."
If departments take a long-term view of the issue, they'll realize that the best approach is to proactively hire a robust support staff, and install enough efficient informatics tools to maximize the efficiency and make practice as enjoyable as possible, he wrote in an e-mail to AuntMinnie.com.
"This is far cheaper in the long run than it would be to lose a critical mass of pediatric radiologists, and then have to recruit new ones," Halsted wrote. "Moreover, a department without such supports in place will find it difficult to retain its newly recruited pediatric radiologists."
Dr. Janet Reid, a pediatric radiologist from the Children's Hospital at the Cleveland Clinic in Ohio, said she is confident that pediatric radiology can be saved.
The most important thing is to attract more residents, she wrote in an e-mail. As for the pluses and minuses of a career in pediatric radiology career, some things about the field simply cannot be changed -- such as the fact that pediatric imaging generally takes longer and that RVU totals will generally be smaller than those generated by adult imaging. At the same time there is hope for more enlightened reimbursement policies that take into account the value of these studies, rather than strict RVU totals, she wrote.
"One solution to the daunting task of increasing the number of pediatric radiologists is to go out and find the residents and let them know about our very exciting field," Reid wrote. "We have done that through pediatricradiology.ccf.org, which is an interactive curriculum available free-of-charge on the Web. Not only does this serve as the key body of knowledge for the radiology resident, it displays the full breadth of our field that includes all modalities, all body systems and deals with a unique set of diseases. The fact that 72 experts from all over the world joined together to compile quality learning material for residents underscores the dedication to teaching and the satisfaction this brings that attracts so many of us to our field."
By Eric Barnes
AuntMinnie.com staff writer
June 14, 2005
Related Reading
Hunting for recruits, pediatric radiologists take aim at "misconceptions," June 26, 2003
Copyright © 2005 AuntMinnie.com