An unusual survey of radiology practices has found that most U.S. facilities are still doing small-bowel follow-through (SBFT) exams. However, only 15% are performing the studies as recommended by the American College of Radiology, raising medical as well as legal concerns.
Survey responses from facilities nationwide confirmed what the researchers already suspected: Most radiologists aren't including fluoroscopic images with compression of all accessible small-bowel loops in their SBFT exams.
The survey was inspired by the anecdotal experience of Dr. Marc Levine, a gastrointestinal radiology specialist at the University of Pennsylvania and lead author of the study. When reviewing SBFT studies from other providers, Levine was often unable to find all the images he wanted to see. Findings from the UPenn survey were published in the online edition of Radiology (March 24, 2004) and will appear in the journal's print edition in May.
The nationwide sample was created by randomly selecting one state in each of nine regions around the country. Surveys were then sent to all chief x-ray technologists listed with the American Registry of Radiologic Technologists in each of those states.
"We chose to survey chief technologists rather than radiologists with the assumption that they are more likely to have a detailed working knowledge of the overall practice patterns of their groups, and are also more likely to provide unbiased data about these practice patterns," the authors wrote.
A total of 452 questionnaires were sent out and 236 were returned -- a 52% response rate comparable to that seen with other similar surveys. Of those 236 facilities, 219 (93%) reported doing SBFT exams.
All of the facilities reported taking a series of overhead radiographs of the patient's barium digestion, although the timing of the series was variable. Fifty-three percent of the 219 groups obtained the radiographs every 30 minutes, 23% at shorter intervals, and 22% at longer intervals.
Almost all of the groups (92%) also obtained spot images of the terminal ileum with each exam, but no fluoroscopy of other small-bowel segments unless the radiographs suggested a problem, the survey found.
"Our findings conflict sharply with the recommendations of the leading experts in small-bowel radiology," the authors wrote. "Our findings also diverge from the ACR standards for performing SBFT studies, which call for fluoroscopic compression of all accessible small-bowel loops with representative radiographs."
Most radiology facilities also aren't performing the enteroclysis exams or peroral pneumocolon exams advocated by small-bowel experts for some cases.
Interestingly, there was no significant difference in the handling of SBFT between academic and private-practice groups. The researchers were also surprised to find that only 19% of the academic groups reported that SBFT exams were performed by GI or abdominal specialists rather than general radiologists.
Meanwhile, the volume of SBFT exams compared to five years earlier was either the same or higher at 62% of the 219 facilities. The researchers noted that while barium studies of the upper GI tract and colon have declined over the years due to competition from endoscopy, SBFT exams are still widely used because of endoscopy's limitations in depicting the small bowel.
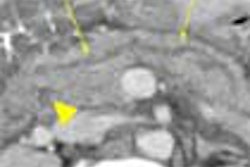
The ACR 2002 guidelines on SBFT reflect a belief among leading specialists that fluoroscopy with manual palpation is needed to better visualize abnormal segments that might otherwise be hidden by overlapping loops on the overhead radiographs.
The medical literature supporting that belief is sparse. One retrospective study of missed small-bowel lesions found that most were overlooked due to technical errors: the lesions couldn't be seen on overhead radiographs and no fluoroscopic spots of the diseased segments had been obtained (Radiology, September 1982, Vol. 144:4, pp. 737-739).
However, Levine and colleagues write that if another study confirms that fluoroscopy makes a difference, "radiologists may need to reassess their policy of relying primarily on overhead radiographs for the evaluation of the small bowel without the benefit of fluoroscopic spot images."
Malpractice expert Dr. Leonard Berlin, chairman of radiology at Rush North Shore Medical Center in Skokie, IL, suggested that radiologists may want to change their practices even sooner.
"If a lesion is missed, and then you look at the exam and see it was not done appropriately -- there was no compression and there are several loops here that aren't visualized -- then the radiologist is going to be liable," Berlin said in an interview with AuntMinnie.com.
By Tracie L. ThompsonAuntMinnie.com staff writer
April 16, 2004
Related Reading
Capsule endoscopy fares well in small bowel versus CT, barium enema, January 14, 2004
Post-toilet cystoproctography pinpoints enteroceles of small bowel, May 9, 2003
Dynamic MR enteroclysis negotiates twists, turns of small bowel disease, February 5, 2003
Given Imaging adds Blue Shield to payor list, February 4, 2003
Video capsule endoscopy deemed superior to small bowel radiography, November 6, 2002
Copyright © 2004 AuntMinnie.com