Sharps injuries occur approximately 800,000 times a year, according to the U.S. Centers for Disease Control and Prevention. The American Nurses Association (ANA) reports that at least 1,000 healthcare workers contract serious infections from needle injuries annually. And the American Hospital Association estimates that one case of serious infection by bloodborne pathogens can quickly add up to $1 million or more in expenditures for testing, lost time, and disability payments.
Between performing biopsies, administering contrast agents, and working in interventional radiology suites, many imaging specialists are at risk for needlestick exposure.
Dr. Judith Weinstein, a New Jersey-based retired interventional radiologist, said she suspects that every interventional radiologist has suffered at least one needle injury.
"Everything we do is via the percutaneous route. Most of these (needles) are pretty long, which increases the risk of someone’s hand being in its way, whether it’s the physician or operator or the assistant. This has a huge impact on the quantity of potential exposures," Weinstein said.
After suffering three needle injuries during her career, Jeannie McFadden, chief radiologic technologist at Bothwell Regional Medical Center in Sedalia, MO, was inspired to develop a transducer sheath that separates the technologist from the needle-guide.
"I have a family, and they pretty much depend on my income to raise them," McFadden said. "What happens if I get a stick here at the hospital and end up with AIDS or hepatitis C and can’t work anymore?"
Since McFadden’s protective sheath was made mandatory in Bothwell Regional’s ultrasound suite, no needle injuries have been reported, said Dr. Robert Farkis, director of medical imaging.
"We certainly feel like we live in a fairly at-risk environment, particularly in ultrasound," Farkis said. "Most of the time we find ourselves working in a dark room because we need to see the screen. We had a couple of incidents here where our technologists got needle injuries, partly because the physicians were trying to watch the screen and put needles in biopsy guides at the same time. You get tied up in the moment sometimes, and I think that’s where the accidents tend to happen."
Needlestick legislation
Needlestick safety has garnered increased attention in the past three years. Nurses’ organizations have led the protection drive, pushing state and U.S. needlestick legislation. Thanks to their efforts, the Needlestick Safety and Prevention Act became effective on April 18, 2001. The act, which is a revision of the 1991 Bloodborne Pathogens Standard, strengthens requirements regarding the use of safety-engineered sharp devices.
The new law requires that healthcare employers document the evaluation and implementation of safety-engineered sharp devices and needleless systems, and review their needlestick-safety control plans annually in light of technological updates. Also, the act requires that healthcare facilities maintain a sharps injury log.
In addition, 34 states have enacted their own needlestick legislation, adding it to their Occupational Safety and Health Administration (OSHA) plans. For example, Missouri passed a law on July 12, 2001 that applies needlestick requirements to state and municipal healthcare facilities that are not subject to federal OSHA standards.
Forming alliances
A group of companies has banded together to form the National Alliance for the Primary Prevention of Sharps Injuries (NAPPSI).
NAPPSI, spearheaded by Venetec International of Carlsbad, CA, aims to advance sharps-injury protection in the healthcare industry through what it calls "primary and secondary needlestick prevention."
Primary prevention involves reducing the need for sharps in the workplace; secondary prevention emphasizes safer sharps practices and technologies. Their main weapon in this fight is the Exposure Prevention Information Network (EPINet). Compiled by the International Healthcare Worker Safety Center of the University of Virginia, Charlottesville, EPINet is a list that categorizes devices by their medical application and suggests a standardized method of recording percutaneous injuries.
NAPPSI has petitioned state governments to distribute the EPINet list to healthcare institutions. So far, three states -- Alaska, Georgia, and Tennessee -- have verbally agreed. The alliance plans to petition the U.S. FDA to do the same, said Dr. Steve Bierman, NAPPSI president and CEO of Venetec.
"What we’re trying to do is, step one, to create in the mind of the physician an awareness that many of the needles (healthcare providers) customarily use do not need to be used. If you must use a needle, use a safety needle. And then, step two, provide a list that makes it very simple for them to access those modalities and implement them in their workplace," Bierman said.
Bierman believes the numbers compiled by the CDC and other safety agencies on needlestick injuries are too low. He cited multiple studies, including ones published by the National Patient Safety Foundation and the Joint Commission on the Accreditation of Health Care Organizations (JACHO), indicating that doctors suffer a 2% needlestick injury rate when suturing. Yet these accidents may be underreported "because they aren’t covered by hospital insurance and (doctors presume) they can handle it themselves," he said.
Prevention
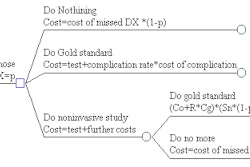
But raising awareness isn't enough. At some point, healthcare providers and their institutions must decide if they're willing to make a financial investment in needlestick prevention.
Although primary and secondary needlestick prevention technologies often cost more than standard products, the base cost is minimal. The American Nurses Association estimates that safe needles cost an average of 28 cents more than regular needles. But if the cost of follow-up surveillance for a high-risk needlestick injury is $3,000 per incidence, the slightly higher cost of safety-engineered and needleless systems is minor, the ANA reported.
StatLock, Venetec’s primary-prevention sterile adhesive anchor for catheters, is an example of a higher-priced, safety-conscious device.
"Suturing takes 12-15 minutes. When you take a StatLock primary prevention securement device, it takes under two minutes. So you return an hour (of procedure time) to the suite. They can do an extra procedure a day. They can generate an extra $1,800 a day. The incremental StatLock cost might be $50," Bierman said.
Alaris Medical Systems of San Diego produces a primary-prevention needle-free IV system called SmartSite, which keeps costs down by reducing the need for caps, cannulae, and add-on components. The SmartSite stand-alone valve costs about $1.25.
While new devices are key to promoting sharps safety, it is the physicians who must take the lead in standardizing needlestick safety. Bierman recommended that institutions start by designating one person to head a safety program, and deciding what primary and secondary prevention modalities to adopt.
NAPPSI offers free membership to healthcare workers, a free monthly newsletter addressing needlestick events and issues, and free lectures on needlestick safety.
"All the pieces are there. Now all you have to do is designate someone to look at it. We know you’re busy," Bierman said. "But put yourself first for a minute."
By Leslie FarnsworthAuntMinnie.com contributing writer
April 19, 2002
Copyright © 2002 AuntMinnie.com