The trend among 21st century women to delay childbearing could lead to an increase in the number of breast cancer diagnoses during pregnancy, which currently stands at about 3,500 annual cases in the U.S.
At the same time, sentinel lymph node (SLN) biopsy and lymphoscintigraphy are becoming the standard of care for these patients. Fortunately, this radiocolloid-based technique doesn't pose significant risk to a fetus, according to research in the Journal of Nuclear Medicine.
The maximum fetal doses that occur during a SLN procedure are "equivalent to the dose received by the mother from about one (day) of natural background radiation in the United States," wrote Dr. Neeta Pandit-Taskar and colleagues from Memorial Sloan-Kettering Cancer Center (MSKCC) in New York City (JNM, July 2006, Vol. 47:7, July 2006).
For this retrospective study, the authors reviewed the records of 1,021 nonpregnant women who underwent SLN mapping and biopsy with injections of Tc-99m sulfur colloid (TSC) for early stage breast cancer at their institution. The patients' median age was 56 years and the median weight was 66 kg. For the 219 women who were of childbearing age, the median age was 40 years. The majority of the women (70.2%) underwent lumpectomy where the TSC injection site remained intact after surgery.
All patients received a single intradermal injection of unfiltered TSC. SLNs were identified with one of two scanning techniques: a one-day protocol (3.7 MBq of TSC) or two-day protocol (18.5 MBq of TSC). The total doses to the injected breast ranged from 5.49 mGy to 14.9 mGy for the two-day protocol. The authors determined the direct absorbed dose from the breast to various organs and also estimated the absorbed dose from systemic TSC in the blood.
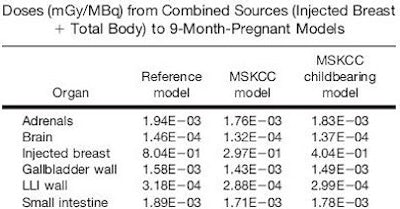
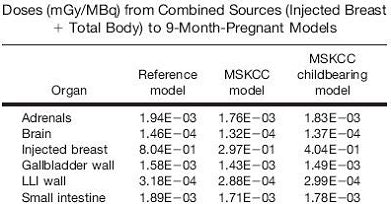
According to the results, the highest estimated absorbed doses were seen for the reference nine-month pregnant model undergoing the two-day protocol: 1.37E-02 mGy for the combined breast-as-source and total body-as-source pathways. The effective doses from the two-day protocol were 0.460 mSv in the reference population, 0.186 mSv in the overall group of women, and 0.245 mSv in the childbearing women (see chart below for organ-based doses).
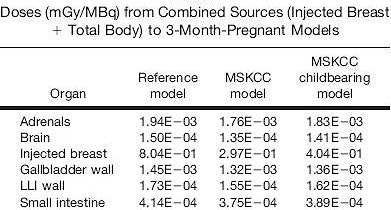 |
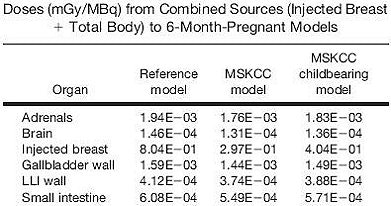 |
| Above and below, partial lists of dose results in three- to nine-month pregnancy models. Reprinted with permission from "Organ and Fetal Absorbed Dose Estimates from 99m-Tc-Sulfur Colloid Lymphoscintigraphy and Sentinel Node Localization in Breast Cancer Patients," Neeta Pandit-Taskar, Lawrence T. Dauer, Leslie Montgomery, Jean St. Germain, Pat B. Zanzonico, and Chaitanya R. Divgi, July 2006, Journal of Nuclear Medicine. |
 |
"Under 'worse-case' conservative assumptions, the maximum estimated fetal exposures reported here (for the 18.7 MBq two-day protocol) are < 3% of the Nuclear Regulatory Commission (NRC) monthly guideline of 0.5 mSv and < 0.3% of the NRC occupations exposure limits during the gestation period of 5 mSv," the authors wrote.
The group's assertion that SLN mapping with TSC can be safely applied during pregnancy is in line with previous research. Five years ago, another group at MSKCC performed a study similar to the current one. In addition to demonstrating the safety of radiocolloid use in this population, they found that a two-day protocol increased patient scheduling efficiency, for nuclear medicine physicians and for the operating room, without compromising the effectiveness of SLN mapping (JNM, March 2001, Vol. 42:3, pp. 420-423).
More recently, surgical oncologists at M. D. Anderson Cancer Center in Houston assessed the risk to the embryo/fetus associated with SNL biopsy and lymphoscintigraphy using about 92.5 MBq TSC in two nonpregnant women with breast cancer. They found that the "maximum absorbed dose to the fetus of 4.3 mGy calculated for the worst-case scenario is well below the 50 mGy that is believed to be the threshold absorbed dose for adverse effects" (Breast Journal, November-December 2004, Vol. 10:6, pp. 492-495).
By Shalmali Pal
AuntMinnie.com staff writer
August 14, 2006
Related Reading
Maternal hyperglycemia at conception linked to fetal cardiohypertrophy, July 26, 2006
Data, not fear, should drive CT decisions in pregnancy, July 10, 2006
Ultrasound and mammography both useful in breast cancer during pregnancy, April 14, 2006
Copyright © 2006 AuntMinnie.com