PET/CT and whole-body MRI appear to be separate but equal when it comes to detecting metastatic disease in breast cancer patients, according to a recent study. Moreover, both 1.5- and 3-tesla scanners successfully detect metastatic and recurrent disease, but with some caveats.
|
Study summary Patients Imaging methods Scan times Readers Results Sensitivity/Specificity |
The German study of 26 breast cancer patients with elevated tumor markers (see Study Summary) found that FDG PET/CT had an edge over MRI for identifying metastatic disease in the lymph nodes, lung, and skin. The research was presented at the 2007 European Congress of Radiology (ECR) in Vienna.
Dr. Gerwin Schmidt, radiologist at the Institute for Clinical Radiology at University Hospitals in Munich, told AuntMinnie.com that morphological scanning can miss many malignant lymph node tumors that are not pathologically enlarged. The study found several patients who had lymph node involvement even though the lymph nodes were smaller than 1 cm.
"With MRI, it can be easy to miss these borderline nodes," he said. "But with PET/CT, their increased tracer uptake makes them appear highly suspicious and made it clear that they were tumors."
PET/CT also showed that several lymph nodes were enlarged due to inflammation and not tumor. When hunting for metastatic lung cancer, PET/CT does not have the problems of motion artifact common with MR scanning. Although these problems have been minimized with more advanced MR technology, some artifacts may still appear due to heart pulsations.
Small melanomas can be easily missed with MRI, but the tracer uptake makes them "jump to your eye" on PET/CT. The study readers were able to detect melanomas as small as 5 mm.
3T protocols need fine-tuning
MRI's proven track record for detecting soft-tissue metastatic disease gave the modality superior marks for identifying brain, liver, and early bone marrow metastatic disease. This superiority held for both 1.5- and 3-tesla scanning, but the protocols for 3-tesla scanning are still being refined.
"We're learning more and more about the capabilities of 3T scanners," Schmidt said. "We're in the privileged position of having both 1.5T and 3T onsite."
An early challenge in the study was developing the imaging protocols for the 3-tesla system; failing to adjust protocols for 3-tesla systems can impair diagnostic quality. Radiologists can't simply apply 1.5-tesla protocols to the more powerful 3-tesla systems. The German researchers had to examine healthy volunteers for image quality, artifact, and clinical analysis. Artifacts appeared on 3-tesla systems that didn't appear on the 1.5-tesla scanners. The STIR and spin-echo sequences were selected because of their high anatomic detail, and their superior ability to differentiate tumor from edema.
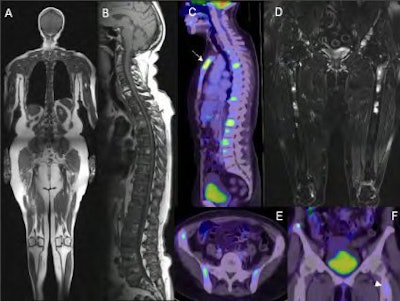 |
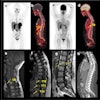
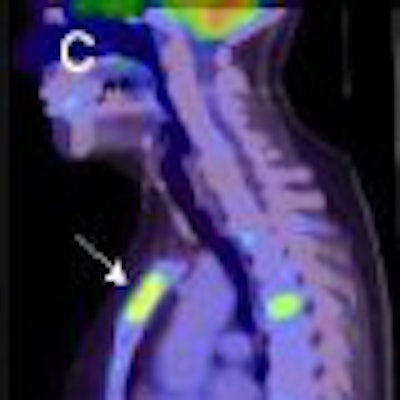
| A 68-year-old woman with breast cancer. A) T1-weighted TSE whole-body MRI at 3 tesla. B) Sagittal T1-weighted TSE sequences reveal infiltration of almost the complete spine. C) PET/CT shows pathological FDG uptake in the larger focal metastases only. A metastasis of the sternum is masked by field saturation and is prone to be missed in peripheral sections of coronal whole-body MRI (arrow). D) Whole-body STIR shows multifocal pelvic metastases and additional infiltration of both distal femurs, an area often not covered by the field of view of the PET/CT scan. E,F) Axial and coronal PET/CT of the pelvis confirms multifocal metastases in both iliac bones. Only faint tracer uptake is observed in a bone metastasis of the left proximal femur (arrowhead). All images courtesy of Dr. Gerwin Schmidt. |
"You need the combined approach -- STIR alone would not work as well," Schmidt said. "The combination of both, even without contrast, is still highly diagnostic for bone metastases, although contrast is vital for organs."
Decisions, decisions
But if PET/CT is better at finding some tumors and MRI is better at detecting others, which one to order? Laboratory and clinical findings generally provide the necessary clues to determine which modality is appropriate, although the choice is further complicated if the radiologist has 1.5- and 3-tesla systems at hand. Schmidt suggested that PET/CT has the biggest impact on primary tumor detection and lymph node staging. To rule out distant metastatic disease in patients who have already undergone surgery and/or chemotherapy, whole-body MRI seems to be the better choice.
In many institutions, the choice falls down to what's available -- if a PET scanner is not onsite, MRI is the default selection. Reimbursement also plays a role -- in Germany, PET/CT scanning is not covered for all patients. Insurance companies are always a bit skeptical of technological innovations, Schmidt observed.
"Most radiologists follow the stepwise approach that has worked for years," he said.
The availability of nuclear medicine physicians is another factor. In Europe, radiologists cannot perform nuclear medicine scanning. To perform PET/CT, a hospital needs either a nuclear medicine physician or a radiologist also certified in nuclear medicine. A shortage of nuclear medicine specialists may pose future problems for PET/CT.
Schmidt and his colleagues would like to expand the study to include more patients (at least 100) and also to encompass patients who have suspicious lab values but are asymptomatic.
"We want to find out what kind of tumor manifestations whole-body MRI would show in patients who develop metastatic disease but who feel completely healthy," he said.
By Brenda Tilke
AuntMinnie.com contributing writer
May 29, 2007
Related Reading
ARRS study: Scintimammography shows high sensitivity in breast cancer detection, May 9, 2007
Mammography still offers advantages over breast MR in DCIS, April 20, 2007
ACS advocates breast MR screening for high-risk women, March 28, 2007
MRI useful for detecting cancer in contralateral breast, March 28, 2007
Whole-body FDG-PET of little use in breast cancer staging, November 26, 2006
Copyright © 2007 AuntMinnie.com