Doctors at William Beaumont Hospital in Royal Oak, MI, do a lot of heart imaging with their dual-source CT scanner. They say they need it because so many of their coronary CT angiography (CTA) patients come from the emergency room with obesity, significant comorbidities, and quite understandably, worries sufficient to keep their hearts racing during the scans.
But aside from a whopping caseload that keeps nine readers busy 12 hours a day, one feature that distinguishes the team at William Beaumont's Ministrelli Center for Advanced Cardiovascular Imaging from other heart centers is the group's emphasis on image quality over other laudable goals.
According to the center director, cardiologist Dr. Gilbert Raff, the focus of the group's protocols on dual-source CT (Somatom Definition, Siemens Medical Solutions, Malvern, PA) is on maximizing image quality for coronary CTA exams, trading off other benefits such as the ability to scan without beta-blockers, or with the lowest possible radiation dose.
In a talk at 2007 International Symposium on Multidetector-Row CT in San Francisco, Raff discussed the patient demographics, processes, and results that led to their current protocols.
CTA challenges
Coronary CTA has always presented challenges for heart imaging, including the need for beta-blockers, the persistence of motion artifacts even at low heart rates, calcium and metal blooming artifacts, and radiation doses of 11-22 mSv, Raff said. The question is whether DSCT can alleviate some or all of these issues.
"One of the things that is a normal challenge for us, if you look at the patients who are coming to the emergency room, is that almost 20% of these patients cannot have beta-blockers, so the heart rate issue is not so simple," he said.
Patients who can't tolerate beta-blockers, such as those with chronic obstructive pulmonary disease or asthma, often present with fast heart rates of 70-80 bpm. For them, DSCT offers substantial advantages in reducing motion artifacts, Raff said. For the other 80% who can tolerate beta-blockade (the group relies on combined oral and intravenous administration of metropolol), DSCT yields higher readability at the same dose.
"Even at low heart rates you don't freeze the motion," Raff said. "Calcium and blooming artifacts from 64-slice, 16-slice, and the previous generation of scanners are obviously quite motion-dependent, and all of these factors combine when you're looking at patients that are excited, upset -- (typical) emergency room patients that have readability issues." With single-source scanners, "we've consistently had somewhere between 10% and 15% of patients" in whom not all segments could be analyzed, he said.
As for the radiation dose of 11-22 mSv, "I am somewhat dismayed that I cannot get the (DSCT) doses down anywhere near some of the ranges that have been proposed academically," he said, and doses have not dropped with DSCT.
Initially the manufacturer believed that radiation doses could be reduced significantly due to reduced diastolic time, Raff said. But the reduction was never realized, in part due to the increased need for late-systolic reconstruction. Another factor, and the most important one, he said, was the group's desire to maximize readability of the segments by combining DSCT with beta-blockers.
"If you take the (high) heart rate as the only criterion for why you want to use DSCT, and you don't have somebody in the cath lab next door coming back and complaining, you might say (you) don't need to use beta-blockers," Raff said.
On the other hand, in a normal practice where patients aren't coming to radiology straight from the emergency department and with serious comorbidities, there's no reason DSCT can't be used without beta-blockers, he said.
But the Ministrelli facility gets large numbers of complex cases, Raff said. And they've been able to markedly reduce blooming artifacts from calcium and stents by using a combination of beta-blockers and DSCT. Owing to a combination of techniques, the group has reduced the percentage of "nondiagnostic" scans from 10% to about 5%, he said.
'Brute force' reconstruction
The final piece of the image-quality puzzle is comprehensive image reconstruction.
"When we inititated our (DSCT) program, we were a little surprised that the best reconstruction wasn't reliably around 60% (of the RR interval) as it used to be with 64-slice CT," Raff said. Conventional reconstructions weren't optimal because individual segments of arteries move differently at higher heart rates. "And there was quite a bit of variation in the exact percentage between one (segment) and the other, and we gave this feedback to the manufacturer," he said.
Siemens responded with a software application called "Best Recon" that more precisely identifies the best diastolic and systolic recons for every lesion. And it works very well, Raff said.
"It will automatically give you the best systolic and diastolic reconstruction, which is frequently not an even number," he said. With this the center has instituted what it calls a "brute force" recon technique that achieves high image resolution by reconstructing multiphase exams at every 10% of the RR interval in a 512 x 512 matrix instead of 256 x 256.
"The result is that we have 10 high-resolution exams to read off of every 10% (of the RR interval)," Raff said. "If you're looking at a lesion in the LAD (left anterior descending artery) and you're trying to get detailed information about the clinical significance of that lesion, you're going to need every trick you've got. So we're pushing the envelope of what you can do. And we literally take each lesion and dial back and forth between, say, 30% ... and 60% recon until we see that particular lesion in the right reconstruction. And when I say lesion, I mean the same artery may have different (optimal) reconstructions at different points."
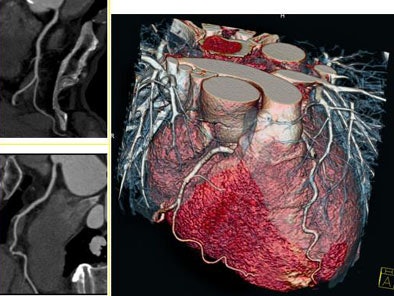 |
| Heart-rate-independent imaging with dual-source CT (DSCT). Coronary CTA images were acquired without beta-blockers at a heart rate 90 bpm. Temporal resolution of 83 msec, spatial resolution of 0.33 mm, six-second scan for 138-mm coverage, 0.33-sec rotation, and 120 kVp. Images courtesy of Nagoya City University Hospital in Japan and Dr. Gilbert Raff of William Beaumont Hospital in Royal Oak, MI. |
High BMI
Obesity is a big problem in Michigan, even more so than in other places. For CT imaging, the extra adipose tissue increases photon scatter and cuts the signal-to-noise ratio. For these patients, the scanner's "CardioObese XXL mode" helps keep more heart images diagnostic by increasing signal to noise at the expense of temporal resolution, Raff said.
The image data is reconstructed over 165 msec -- so there is duplicate data from the second one-quarter gantry turn. "Basically, instead of doing a quarter-scan recon on the patient, we're doing a half-scan recon, and thereby increasing the signal-to-noise ratio in these patients' scatter," he said, noting that the method has enabled diagnostic scans in patients over 50 BMI.
"We think the main reason DSCT should be thought of as a good tool is because it improves image quality," Raff said. There are virtually no reconstruction or stairstep artifacts, "and beta-blockers are optional, so for patients with heart and lung disease you can optionally eliminate it," he said, though CTA without beta-blockers has not turned out to be the best approach for most of the group's cardiac imaging patients. Finally, Raff said, "the best reconstructions require a special approach."
By Eric Barnes
AuntMinnie.com staff writer
October 8, 2007
Related Reading
High-speed CT useful for evaluating coronary disease in symptomatic patients, August 14, 2007
Coronary CTA results correlate with all-cause mortality, June 19, 2007
Dual-source coronary CTA images the calcium-burdened, April 13, 2007
Dual-source imaging promises better CT scanning, June 15, 2007
Siemens launches new dual-source CT technology, November 17, 2005
Copyright © 2007 AuntMinnie.com