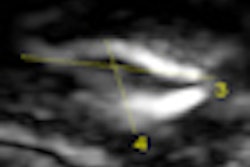
A new study released today in the Journal of the American Medical Association indicates that a single negative compression ultrasound scan of the entire leg may be good enough to rule out deep vein thrombosis (DVT), avoiding the need for multiple follow-up imaging studies.
The findings suggest that clinicians may be able to withhold anticoagulation therapy after a single negative scan, with a less than 1% chance that a patient might develop a blood clot over the next three months. The findings were reported by a research team led by Dr. Stacy A. Johnson from the University of Utah in Salt Lake City (JAMA, February 3, 2010, Vol. 303:5, pp. 438-445).
Standard of care
Current standard of care for patients with suspected proximal deep vein thrombosis (above the knee) is to perform compression ultrasound, but the modality's accuracy for distal DVT (below the knee) has been questioned, according to the authors. The problem is that up to 25% of distal DVTs can migrate into the proximal veins, increasing the risk of pulmonary embolism.
If a patient has a negative compression ultrasound scan, current practice guidelines call for serial studies of the proximal veins five to seven days after the initial study to rule out clinically suspected DVT. But the authors questioned the cost-effectiveness of this technique, since only 1% to 2% of repeat compression ultrasound scans detect propagation of the thrombus. Another problem is that many patients do not return for follow-up scans.
One solution is to use a single whole-leg ultrasound scan of both the proximal and distal veins to exclude DVT and reduce the need for repeat follow-up tests. However, there are concerns about whether it's advisable to use a single exam following an initially negative result, especially in patients with a high pretest probability for DVT.
To examine the question, Johnson and colleagues performed a meta-analysis of seven studies published from 2003 to 2010, totaling 4,731 patients who did not receive anticoagulation therapy because they had negative initial whole-leg compression ultrasound exams. The patient population included 647 patients (13.7%) who had active cancer and up to 725 patients (15.3%) who had recently undergone a major surgery.
The researchers calculated the event rate for confirmed venous thromboembolism at the three-month follow-up point, and also calculated the rate for deaths attributable to venous thromboembolism, and pooled the results for all seven studies. They also calculated event rates for different subgroups in the patient population, such as high-risk patients versus those at low risk.
Of the 4,731 patients who met the study criteria of having anticoagulation therapy withheld due to an initial negative whole-leg ultrasound exam, researchers found 34 cases (0.7%) of either confirmed venous thromboembolism or death attributable to venous thromboembolism. Of these patients, 11 had distal DVT, seven had proximal DVT, seven had nonfatal pulmonary embolism, and nine patients died.
The researchers also found that individual rates of venous thromboembolism incidence in the seven studies ranged from a low of 0.24% to a high of 1.95% at the three-month follow-up interval, with the studies producing a pooled incidence rate of 0.57%. Across different risk groups, the researchers found a pooled venous thromboembolism incidence rate of 0.29% for low-risk patients, 0.82% for moderate-risk individuals, and 2.49% for high-risk patients.
Low incidence rate
In analyzing their findings, the researchers reported that the incidence rate of 0.57% for venous thromboembolism indicated that patients who were denied anticoagulant therapy on the basis of an initial whole-leg ultrasound exam were at low risk for negative events. They also noted that the death rate from suspected venous thromboembolisms (nine patients or 0.19% of the total) might be overreported because all of these patients were acutely ill, and none received necropsies that objectively confirmed thromboembolism as the cause of their deaths.
"Withholding anticoagulation following a single negative whole-leg CUS [compression ultrasound] result was associated with a low risk for venous thromboembolism during three-month follow-up in patients with suspected DVT," the authors stated. "The efficiency and convenience of whole-leg CUS as a single study is superior to that of repeated CUS evaluations."
There could be some drawbacks, however, if whole-leg ultrasound became the standard of care for diagnosing distal DVT, the authors cautioned. Many distal thrombi appear to resolve without the use of anticoagulant therapy, and some might argue that diagnosing and treating distal DVT is unnecessary because it might place patients at risk of anticoagulant-related complications, such as a 1.1% risk of major bleeding.
In a related commentary in JAMA, Dr. Robert McNutt, Ph.D., of Rush University Medical Center in Chicago and Dr. Edward Livingston of the University of Texas Southwestern Medical Center in Dallas cautioned against using summary statements from a meta-analysis study to guide patient care.
"Such conclusions are not helpful when the clinical studies are combined and averaged in a way that reduces the complex world of medical care to overly simple and consequently not clinically useful statistical summaries," they wrote. "Meta-analyses are most appropriately used to formulate, but not test hypotheses."
By Brian Casey
AuntMinnie.com staff writer
February 2, 2010
Related Reading
Limits on off-hours DVT ultrasound may be more efficient, November 5, 2009
Two-point US exam keeps up with whole-leg US in detecting DVT, October 9, 2008
Lack of residual vein thrombosis indicates low risk for recurrent DVT, September 17, 2008
Rapid lysis technique removes DVT, prevents post-thrombotic syndrome, March 5, 2007
New venous thromboembolism diagnosis guidelines specify imaging's role, February 16, 2007
Copyright © 2010 AuntMinnie.com