Talk about poor access to healthcare. Astronauts aboard the International Space Station (ISS) are never closer than 250 miles from the nearest doctor. And that first step toward the hospital could only be described as breathtaking.
But help is on the way. Call it a new mobile imaging center. Doctors and engineers at the National Aeronautics and Space Administration (NASA) have designed a remotely guided teleradiology system and imaging template that allows lay persons to perform genitourinary ultrasound procedures on their colleagues in space.
 |
| Since Russia launched the first component on November 20, 1998, the International Space Station has become an enduring symbol of international cooperation. The ISS orbits at a height of 250 miles above the earth, at a speed of more than 5 miles per second. The orbiting scientific laboratory now includes 16 components and measures 171 feet long, 240 feet wide, and 90 feet high, with 15,000 cubic feet of living space, with a mass equal to 415,209 pounds. Once completed, the ship's mass will increase to nearly a million pounds, and its scientific capabilities are expected to grow accordingly. All still and video images courtesy of The National Aeronautics and Space Administration (ISS tracking service available at "Science at NASA"). |
Space is the place for genitourinary problems
Genitourinary imaging seemed a logical place to start because of the particular health risks encountered in space, said Dr. Jeffrey Jones, NASA's lead flight surgeon for the ISS, in a talk at the 2004 American Urological Association meeting in San Francisco. He provided additional details in follow-up interviews with AuntMinnie.com.
To begin, exposure to microgravity conditions generally increases the risk of urolithiasis, and has resulted in at least one acute in-flight episode, Jones said. In fact, the group has identified 30 genitourinary conditions that could potentially cause problems in space flight, most related to stones, urinary retention, and urinary-tract infections, Jones said.
"We had the goals of improving our medical support in case of harm, illness, or injury, improving our diagnostic abilities, and thereby lowering the probability of unnecessary medical deorbit or evacuation of the space station," he said.
The system requirements for an on-board imaging unit were, in a word, astronomical. First the equipment would have to transmit diagnostic-quality grayscale images back to Mission Control in Houston without disrupting other vital communications between the shuttle and its earthbound support team. And it would have to do so in real time, using untrained personnel as operators, and under audio guidance from earth.
"Unfortunately we did not have a trained ultrasonographer on board the space station, so we had to test the paradigm of using remote guidance to acquire digital images," Jones said. "We used a three-step approach to do validation of our protocols: We started off with a remote environment ground-based scenario, we proceeded to a zero-gravity test-phase scenario, and then we tested the protocol onboard (the space station) itself."
An ancient crater on Devon Island in the Canadian Arctic made "an excellent analog for our ground search operations," Jones said. "It's cold, dry, rocky, uninhabited, and isolated, the meteor impact is approximately 20 million years old…(and) very well preserved, much like you see on the planet surface of Mars." (More information about the island can be found at http://www.marsonearth.org/.)
By the time the ultrasound equipment had been unloaded at the crater, scientists had already tested the communications protocol, developed at the Jet Propulsion Laboratory in Pasadena, CA. The experiment used a signal from a modified ATL HDI 5000 ultrasound scanner (Philips Medical Systems, Bothell, WA), which was uplinked to a NASA Advanced Communications Technology Satellite (ACTS) and then back down to Mission Control in Houston, using bidirectional 128, 256, and 384 kbps satellite links (Journal of Digital Imaging, May 1999, Vol. 12:2, pp. 68-76).
The protocol was similar on Devon Island, except that the ultrasound images came from a portable ultrasound scanner (SonoSite 180, SonoSite, Bothell, WA). This time the images were uplinked to the ACTS satellite and then back down to Mission Control, Jones said.
"Next we went to the operation flight scenario with a KC-135 aircraft, taking advantage of its unidirectional video and bidirectional audio communication capability," Jones said. Both the ATL and the Sonosite scanners were used on the aircraft. "The image quality is a little better with the ATL, but you're still able to get diagnostic-quality images with the SonoSite, and the SonoSite is much more portable," he said.
"The KC-135 generates zero gravity during parabolic flight, and during the ascending and descending phases there's approximately 30 seconds of freefall which simulates microgravity, and we can test a whole variety of operation scenarios aboard the aircraft… We took the 40-60-parabolas flight test during a single flight. This aircraft is not nicknamed 'the vomit comet' for nothing."
 |
| ISS-5 crew surgeon Dr. Jeffrey Jones after the flight from Houston to Cape Kennedy prior to the launch of his crew on the NASA STS-111 mission to the International Space Station. |
In the simulated microgravity experiment, ultrasound images from a porcine model (they apparently do fly) were uploaded to the ACTS satellite, and then downloaded successfully back to Mission Control, according to Jones.
Liftoff
Now it was time for the real thing. The astronauts underwent two hours of training on the ultrasound system and an hour of learning how to scan the genitourinary system. Scanning was further simplified by the use of imaging templates in the form of matching cue cards in Houston and on the spacecraft, with the scanning directed by Dr. Ashot Sargsyan, ISS ultrasound project medical lead, Wyle Laboratories. (Wyle, of El Segundo, CA, is the prime contractor for the Space and Life Sciences Directorate at NASA's Johnson Space Center.)
"The cue card has the body kind of partitioned up by alphabet and numbers, and we would say 'put the probe in the B-1 position,' Jones said. "And the B-1 position corresponds with a specific anatomic location, so they just go right there, and we say 'now tilt the probe towards the head' -- we use standard terminology we trained them on pre-flight -- and they can then tilt the probe to get the right image."
ISS crew member Peggy Whitson, who holds a Ph.D. in physiology, was chosen to undergo training and perform the scans on the space station. Sargsyan directed the scanning from Houston by voice.
 |
| Crew member Peggy Whitson, Ph.D. conducts the ultrasound exam on herself aboard the ISS. |
"We used a C52 tubular curved-array broadband probe with 640 x 480-pixel spatial resolution and 7.5 frames per second temporal resolution (on the ATL scanner)," Jones said. The relatively low resolution, combined with six-bit grayscale, was designed to provide reasonable image quality without impeding the ship's other communications functions. The space station's entire video downlink bandwidth is equivalent to approximately 30 frames per second, leaving about 32.5 fps available for other purposes.
Multiple data conversions can sometimes degrade image quality, ultrasound project leader Sargsyan explained in an e-mail to AuntMinnie.com.
"The analog output of the ultrasound system is converted into a data stream, downlinked by means of a NASA TDRSS satellite, and then 'reassembled' into an analog video signal," Sargsyan wrote. "It is then routed to a building at the (Johnson Space Center) and recorded on a tape." The resulting images can show some minor degradation in quality, however, these are strictly a result of the conversions and not the teleradiology process, he explained.
See and hear ultrasound in space
Note: Be sure to turn on your speakers to hear the audio tracks in videos two through five. In order to play the .wmv files linked below, you will need to have installed a media player such as the Windows Media Player (download) or the RealPlayer (download).
Video 1: Once in orbit on the ISS, Peggy Whitson, Ph.D., tests out the ATL 5000 scanner on ISS increment 5 commander Valery Korzun, ensuring that the cables are long enough to conduct the exam (no audio).

Video 2: Remotely guided imaging on orbit demonstrating the potential pleural space, and the lung sliding over the parietal pleura. On the audio track, Sargsyan directs the exam remotely from Houston to the ISS.


Video 3: A fragment of the remotely guided imaging on orbit demonstrating a ureteral jet on the left side; urine (pink) seen in Doppler US flows from the ureter into the bladder. This exam assumes more importance in space as ultrasound is the sole modality available to assess ureteral patency. On the audio track, Sargsyan directs the exam remotely from Houston to the ISS.


Video 4: Splenorenal potential space as a component of the guided FAST exam. On the audio track, Sargsyan directs the exam remotely from Houston to the ISS.


Video 5: US of right upper quadrant; right kidney and liver are visible. On the audio track, Sargsyan directs the exam remotely from Houston to the ISS.


 |
| Sleep-deprived but celebratory, the Houston medical team poses immediately after successfully completing of ultrasound experiment. From left to right: medical operations clinician Dr. Douglas Hamilton (Wyle Laboratories); scientist (Physiology) - Victor Hurst, Ph.D. (Wyle Laboratories); NASA lead flight surgeon for ISS, Dr. Jeffrey Jones (NASA, Johnson Space Center); scientist (ultrasound) David Martin, RDMS, RDCS (Wyle Laboratories); ISS ultrasound project engineering lead Shannon Melton (Wyle Laboratories); ISS Ultrasound project medical lead, Dr. Ashot Sargsyan (Wyle Laboratories). |
Gauging image quality
Following the successful experiment, a retrospective study was undertaken to assess image quality. Six radiologists experienced in ultrasound interpretation subjectively compared the quality of ground-based images against those acquired in space and sent down to Houston, grading the images on a scale of one to seven. Each reader examined two sets of images in each of seven anatomic regions in the urinary tract. Only normal anatomy was found in all of the subjects; astronauts undergo extensive ultrasound screening as part of their preflight medical workup.
"We separated them into renal size, shape, contour, renal parenchyma, renal arteries, renal veins, calyces, the bladder, and bladder wall, and we scored each one individually…. So we were comparing one (anatomic) region in 0 G to one region in 1 G," Jones said.
The difference in the image-quality scores, 5.8 overall for the terrestrial images versus approximately 5.6 for the space-based pictures -- was statistically insignificant except in the renal vein images.
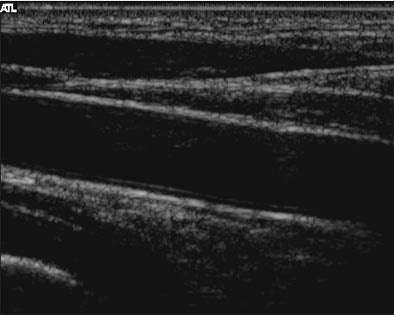 |
| A full-resolution fragment of a carotid artery image, one of many stills downlinked from the ISS post-examination. |
"There were slightly diminished scores for zero gravity, but most of them weren't statistically different from the 1-G images," he said. The delay from the time the images were transmitted until they were received in Houston varied from approximately 1.5 to 3.5 seconds for the experiment.
 |
| A transverse scan at the level of the left renal vein, captured post examination from the recorded video. In spite of degradation due to conversions, the image offers ample imaging data. |
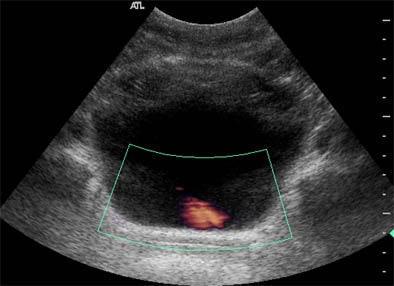 |
| Remotely guided Doppler ultrasound of the left ureter shows urine flow (pink) into the bladder. |
"None of the in-flight (transmission) times were significantly different from those that we acquired in pre-flight reception. We felt that these images were for the most part diagnostic," Jones said. The limitation of the study is that it compared ultrasound to ultrasound, without further confirmation of the (normal) findings, he added.
"I think this imaging test has provided the proof of the pudding, as they say, with the use of a diagnostic noninvasive nonionic imaging tool on the ISS," Jones concluded. "I think we have some limitations, but I think this technique will provide diagnostic images to enable crew surgeons on the ground to make informed recommendations about the assessment of crew members for space flight."
The technique is potentially applicable on Earth as well, he added, perhaps in an isolated setting where no physician is available.
By Eric BarnesAuntMinnie.com staff writer
July 30, 2004
Related Reading
Space
station technique expands use of ultrasound, March 31, 2004
Ultrasound aces search for ureteral stones, March 7, 2004
US combo boosts detection, characterization of perianal inflammation, January 15, 2004
Prevoiding transabdominal sonography clears way for uroflowmetry, October 14, 2003
Dynamic US offers high sensitivity for pediatric bladder exam, July 28, 2003
Copyright © 2004 AuntMinnie.com