Researchers have found that a prenatal diagnosis of vasa previa -- an obstetrical condition that historically resulted in 95% fetal mortality -- can reverse expected outcomes to achieve nearly 100% fetal survival.
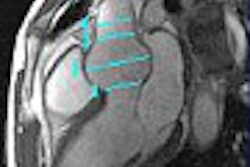
Prenatal ultrasound exams with color Doppler imaging can easily check for this rare but critical condition, according to a presentation at the 2004 American Institute of Ultrasound in Medicine (AIUM) meeting in Phoenix.
"I cannot think of any other condition where prenatal diagnosis makes such a difference between survival and death," said presenter Dr. Yinka Oyelese, a maternal-fetal medicine specialist from the Robert Wood Johnson Medical School in New Brunswick, NJ.
Vasa previa occurs when placental or umbilical blood vessels traverse between the fetus and the cervix. As the cervix dilates or the membranes over it rupture, the unprotected blood vessels can tear, causing rapid fetal hemorrhage.
If diagnosed prior to labor, a pregnant patient is advised to undergo an early cesarean delivery to avoid spontaneous rupture of the blood vessels.
Excluding vasa previa, by checking for normal insertion of the umbilical cord into the placenta, can be routinely and easily incorporated into prenatal ultrasound exams, Oyelese said.
 |
| Vasa previa can be diagnosed by transvaginal color Doppler ultrasound, as shown on this image. Image courtesy of the International Vasa Previa Foundation. |
In one study of 667 pregnant patients, identifying the placental cord insertion took an average of less than 20 seconds. In 95% of cases it took less than a minute (Ultrasound in Obstetrics and Gynecology, December 1998, Vol.12:6, pp. 426-429).
In the estimated one of every 2,500 pregnancies involving vasa previa, however, a diagnosis prior to maternal labor can make all the difference, according to the latest research.
Oyelese and researchers from five other centers partnered with the Boca Raton, FL-based International Vasa Previa Foundation to identify sufficient cases for a statistically robust study. Their study currently includes 155 cases of vasa previa verified by pathology or photographs.
Of those 155 vasa previas, 61 were diagnosed prenatally and 94 were not. Among the prenatally diagnosed cases, 97% of the infants survived; in the undiagnosed cases only 44% survived.
According to another outcomes measure, 67% of the neonates born with undiagnosed vasa previa required a blood transfusion, compared with only 5% of those with prior diagnosis.
Most of the diagnosed cases were only identified because the patient also had a placenta previa, Oyelese said. Researchers believe a low-lying placenta may precede vasa previa.
The risk factors for vasa previa appear to be:
- Low-lying placenta or placenta previa in the second trimester, regardless of whether it remains low-lying at delivery
- Succenturiate or bilobed placenta
- Velamentous cord insertion
- In-vitro fertilization pregnancy
- Multiple pregnancies
- History of uterine surgery or D&C (dilation and curettage)
- Painless bleeding
In an earlier report on their findings, the researchers suggested that women at increased risk be examined with transvaginal color Doppler sonography in the region over the cervix if vasa previa cannot be excluded by transabdominal sonography.
The group also recommended that women with diagnosed vasa previa undergo elective cesarean delivery at 35 weeks, or earlier if fetal lung maturity is documented (Obstetrics & Gynecology, May 2004, Vol. 103:5, pp. 937-942).
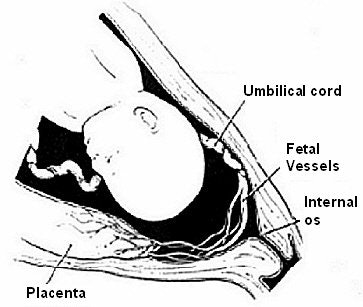 |
| Vasa previa occurs when one or more of the placental or umbilical blood vessels cross the entrance to the birth canal beneath the fetus. Drawing courtesy of the International Vasa Previa Foundation. |
Diagnosed patients should be hospitalized if contractions or blood spotting occurs, and steroids to promote fetal lung maturation should be considered, they added.
"It is our opinion that the mild risks associated with prematurity at 35 weeks of gestation are outweighed by the risk of a dismal outcome should the membranes rupture, especially because approximately 80% of women at term will have ruptured membranes at the onset of labor," the authors wrote.
Not all cases of vasa previa are necessarily recognizable with sonography, the authors cautioned, citing factors such as abdominal wall scarring, maternal obesity, or an incompletely filled maternal bladder that may prevent visualization of the cord entry.
Vessels that course over the cervix transversely rather than anteroposteriorly may also be missed by transabdominal color Doppler ultrasonography, the researchers wrote.
But incorporating a cord check into routine prenatal ultrasound is absolutely worthwhile. "If the cord insertion is normal and you don't have a low-lying placenta, you can virtually rule out vasa previa," Oyelese told the AIUM audience.
By Tracie L. ThompsonAuntMinnie.com staff writer
July 14, 2004
Related Reading
Sonographic sign reliably excludes ectopic pregnancy, June 22, 2004
Noninvasive prenatal testing cuts amniocentesis use, June 1, 2004
PCI bears no relationship to preterm delivery, July 24, 2002
Copyright © 2004 AuntMinnie.com