Minor sonographic markers can play a major role in determining whether invasive testing should be recommended in pregnant women. They can help lower risk or reinforce the requirement for invasive testing.
Using sonographic markers to modify the risk of chromosomal abnormality, also known as a genetic sonogram, has become more of a necessity in recent years. As the average age of women having babies goes up, using age alone to quantify risk and offering invasive testing based on age become impractical.
Also, it is inaccurate to ignore other variations that are independent of age while calculating risk. If, for instance, age is used as the sole criteria to quantify risk for Down syndrome, only 30% of cases can be identified. About 70% of Down syndrome fetuses occurring in women under the age of 35 will be excluded from testing.
Minor markers
In a paper presented at the Clinical UltraSonography in Practice (CUSP) conference in Chennai, Dr S. Suresh and Dr Madhukar Pai explained the significance of minor markers in evaluating risk for chromosomal abnormalities. Suresh is the director of Mediscan Systems Diagnostic Ultrasound Research & Training Centre in Chennai, and Pai is a doctoral candidate at the University of California, Berkeley.
"One approach to screening is to determine the pretest probability using maternal age, history, and maternal serum screening. This estimate of pretest probability is then revised using the results of the genetic sonogram," Pai said.
Suresh explained the significance of the choroid plexus (CP) cyst, increased nuchal fold thickness, echogenic intracardiac foci, echogenic bowel, and pyelectasis among the minor markers associated with fetal aneuploidy.
Significance of isolated markers
CP cysts over 3 mm in size are taken to be markers. Like other markers, they can also be found in normal fetuses, but are more often found in aneuploid fetuses.
In a series of 27,511 second-trimester scans, Suresh found a 0.7% occurrence of CP cysts. About 65% of them were bilateral, while 35% were unilateral. About 82% were isolated, and 18% were associated with other anomalies.
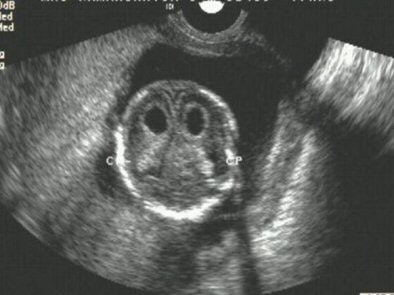 |
| Bilateral choroid plexus cysts. All images courtesy of Dr S. Suresh. |
"If the CP cyst is isolated and the patient is otherwise at low risk for fetal aneuploidy, there is no need to offer modified standard obstetric management or offer invasive testing in the antenatal period," Suresh wrote in his paper.
Similarly, hyperechogenic bowel is viewed as a normal variant in the second trimester when it is not associated with other ultrasound findings. About 10% of Down syndrome cases show hyperechogenic bowel.
Ultrasound can show diffuse increase in echogenicity of the small bowel, focal increase in echogenicity, or bowel echogenicity equal to that of the bone. The last appearance of the hyperechogenic bowel has the greatest association with adverse outcome.
Hyperechogenic bowel increases risk for aneuploidy 5.5 times.
The third marker, mild renal pyelectasis, usually resolves after birth. About 2% to 3% of normal population are also likely to have pyelectasis. However, this is an important marker given that 17% to 25% of Down syndrome cases have hydronephrosis.
The kidneys are imaged in the transverse plane and measured in the anteroposterior plane. If the diameter is greater than 7 mm at 30-40 weeks, there is an increased risk of Down syndrome.
 |
| Renal pyelectasis. |
Variation with ethnicity
At times ethnicity can have a significant bearing on the weightage given to a marker, as is the case with echogenic intracardiac foci (EIF). "The incidence of EIF in Asian mothers is higher than those seen in fetuses with Down syndrome.... In low-risk women, the presence of EIF does not warrant further testing, especially in Asian population," Suresh said.
EIF is commonly observed as a single focus in the left ventricle.
 |
| Echogenic intracardiac focus (arrow). |
As compared to the CP cysts and hyperechoic bowel, EIF is a fairly common finding at 3% to 10% of the population. However, less than 20% of aneuploid fetuses have EIF. Chances of aneuploidy are greater if EIF is seen in both ventricles.
Markers with high sensitivity
Nuchal fold thickness is the first sonographic marker to have been associated with increased risk of Down syndrome. An increased nuchal fold thickness of 6 mm or higher warrants a fetal karyotype, regardless of associated abnormalities, Suresh said. The nuchal fold thickness should be measured only between 15-20 weeks because the normal skin thickness remains unchanged in this period.
For measuring nuchal fold thickness, a transaxial view of the head is taken through the thalamus, cerebellum, and occipital bone. The nuchal fold thickness is measured in the cerebellar plane from the outer surface of the occipital bone to the outer surface of the skin.
 |
| Increased nuchal fold thickness. |
The following table shows how risk for Down syndrome changes depending on whether the ultrasound shows normal or increased nuchal fold thickness in the fetus.
|
||||||||||||||||||
| Courtesy: Dr Suresh, CUSP | ||||||||||||||||||
"The most important minor marker is the nuchal fold. Short humerus and echogenic bowel are the second most important markers. EIF, renal pyelectasis, and CP cysts have poor accuracy and limited impact on Down syndrome," Pai said.
The following table lists the likelihood ratios of the markers as given by different studies.
|
|||||||||||||||||||||||||||||
| Courtesy: Dr Madhukar Pai, CUSP | |||||||||||||||||||||||||||||
"Minor markers cannot replace karyotype diagnosis by invasive testing, but (they) can definitely reclassify a high-risk patient as low-risk and vice versa," Suresh concluded in his paper.
By N. Shivapriya
AuntMinnieIndia.com
October 19, 2004
Related Reading
Moving beyond sensitivity and specificity, October 13, 2004
Copyright © 2004 AuntMinnie.com