Is it groundbreaking public policy or a case of the law outpacing the clinical evidence? Either way, the eyes of Texas are following the potential impact of new legislation that will take effect on September 1 requiring insurers to pay for CT and ultrasound scans for atherosclerosis screening.
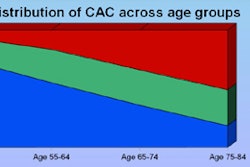
The Texas Heart Attack Prevention Bill (HB 1290) mandates that all health benefit providers in the state provide a minimum of $200 per individual every five years to cover the cost of CT coronary artery calcium (CAC) scans or carotid ultrasound studies. The coverage must be offered to men between the ages of 45 and 76 and women between the ages 55 to 76, as well as anyone else who has diabetes or is deemed to be at intermediate risk or higher for developing coronary artery disease per the Framingham risk score.
The controversial bill (click here for complete text in PDF file) was signed into law by Gov. Rick Perry on June 23. The first of its kind in the U.S., it was passed in early June by both houses in the Texas Legislature after being introduced twice and withdrawn once. Filed by Rep. René Oliveira (R-Brownsville) on his first day back at work from coronary artery bypass surgery, the legislation was modeled on the Screening for Heart Attack Prevention and Education (SHAPE) task force guidelines published in 2006, in which the Society for Heart Attack Prevention and Eradication (also SHAPE) of Houston recommended screening of all individuals at risk of a heart attack.
Despite the bill's passage, it remains controversial for several reasons. First, the law mandates coverage of broad-based screening, requiring the use of radiation in the case of CAC scans (although such tests are now commonly performed using less than 1 mSv of radiation).
There are also concerns that the yield of positive results per capita -- in terms of individuals identified through screening who would then have an opportunity to undergo treatment or make lifestyle modifications -- remains insufficient to justify the expenditure. Finally, critics of the new law are concerned that a large influx of new patients showing up for screening could overburden the healthcare system, and that downstream testing of incidental findings could add substantially to both risks and the cost of care.
A hot potato?
Perhaps because of these issues, support for the nascent law is something of a hot potato, to the point where some individuals contacted by AuntMinnie.com were unwilling to comment. The American Heart Association (AHA), the American College of Cardiology, the American College of Radiology, and the Texas Radiological Society all take no official position on the legislation. A prominent Texas radiologist declined to speak on the record, saying only that expressing either support or opposition to the law would be too controversial.
The Texas Medical Association told AuntMinnie.com that it "monitored" the bill in the Texas Legislature without taking a position. Helen Kent Davis, director of governmental affairs with the Austin-based association, said the organization rarely supports preventive care with a few exceptions. As for the new bill, the physicians on the scientific committee felt that mandatory screening was "too expensive for widespread use."
The American Heart Association's vice president of advocacy, Joel Romo, said that the lack of an endorsement now doesn't mean one won't eventually be produced, merely that the process is slow. All of the AHA's policy positions involve a painstaking, collaborative process "based on hard science and the unanimous approval among policy committees made up of our volunteers across the country," Romo told AuntMinnie.com. "For this particular issue, we just didn't have anything from the AHA that could give us a conclusive position whether it was for or against."
Shaping legislation
On the other hand, the Society for Heart Attack Prevention and Eradication has been a major proponent of the legislation throughout its ups and downs in the Texas Legislature, stating on its Web site that the results of the group's analysis found that proper screening of the asymptomatic men and women of screening age could:
- Prevent more than 4,300 deaths from cardiovascular disease each year in the state (more than 90,000 deaths in the U.S.).
- Reduce the Texas population with a history of heart attack -- currently estimated to be 550,000 -- by as much as 25%.
- Save approximately $1.6 billion annually (more than $21 billion in the U.S.).
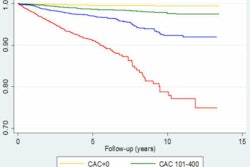
Dr. Matthew Budoff, a SHAPE task force panel member and an assistant professor of cardiology at Harbor-UCLA Medical Center in Los Angeles, defended the organization's support of the law, telling AuntMinnie.com that the data are "overwhelming that calcium scoring is the best current known predictor of future cardiovascular events in asymptomatic persons" and support the Texas law.
Although the AHA may not endorse it, the organization does support the use of calcium scoring for intermediate-risk patients, per its 2006 statement on cardiac CT, wrote Budoff, first author of the 2006 AHA report, in an e-mail.
The Multi-Ethnic Study of Atherosclerosis (MESA) (New England Journal of Medicine, March 27, 2008, Vol. 358:13, pp. 1336-1345), a 6,814-person National Institutes of Health-funded study showed that calcium scoring was the best predictor of cardiac events, better than C-reactive protein, intimal-medial thickness (IMT), and traditional risk factors, Budoff wrote. Finally, new five-year follow-up results of the Heinz Nixdorf Recall Study presented at the 2009 American College of Cardiology meeting "also strongly show that calcium scoring was a better predictor of events than risk factors, and strongly support the law," he wrote.
SHAPE chairman Dr. Morteza Naghavi last year responded to criticism that the science was not yet sufficient to support population-wide atherosclerosis screening -- and that any false-positive results could actually be dangerous if they led to unnecessary additional tests -- by arguing that CAC scoring would be useful in identifying more individuals at risk of heart attack.
"Most initial myocardial infarctions occur in asymptomatic individuals with unrecognized atherosclerosis who are classified by the Framingham risk score as low or intermediate risk," Naghavi and colleagues wrote in a letter to the Journal of the American Medical Association. "Thus, when screening is based on risk factors alone, most individuals destined for a near-term myocardial infarction are not identified and, consequently, not offered adequate preventive treatment" (JAMA, May 14, 2008, Vol. 299:18, pp. 2147-2148).
Dr. Pamela Bowe Morris, director of the Seinsheimer Cardiovascular Health Program and co-director of the Women's Heart Care Program at the Medical University of South Carolina in Charleston, told AuntMinnie.com that she also strongly supports the new law. The evidence favoring both CAC scoring and carotid artery sonography is compelling, and the need for increased screening is real, she wrote in an e-mail.
"There is a strong multiethnic evidence base in men and women that both assessment of coronary artery calcification (calcium scoring) and measurement of carotid intima media thickness (carotid IMT) can improve our ability to identify individuals with subclinical atherosclerosis who are at risk for future cardiovascular events," Bowe Morris stated. "Current guidelines recommend initial risk stratification based on risk scoring algorithms such as the Framingham risk score. However, many individuals fall into an 'intermediate risk' range, and the need to pursue aggressive preventive therapies may be uncertain. It is in just such patients that noninvasive imaging for the presence of already-present subclinical disease can greatly aid physicians as they design a preventive regimen and determine the intensity of treatment."
Until now these simple and noninvasive tests have been available only to more financially advantaged patients who can afford to pay for the tests out of pocket, Bowe Morris wrote. "With the great groundbreaking decision of the Texas Legislature, all insured appropriate individuals in the great state will now be able to benefit from this advanced technology and improved cardiovascular risk prediction," she stated. The decision "shows great appreciation for the devastating morbidity and mortality that is caused by cardiovascular disease ... and the need to be more aggressive in identifying persons at risk and implementing aggressive preventive strategies."
Dr. Raymond Stainback, a supporter of the bill and a councilor with the Texas chapter of the American College of Cardiology, spoke to Heartwire about the act in June. The law's provisions are generally considered reasonable, he told the publication, and the tests are already in common use today -- but purchased entirely at the patient's expense.
"In some cases, the doctor may feel that an additional piece of concrete imaging screening data would be helpful for encouraging aggressive and sometimes expensive-for-the-patient preventive measures, such as statin therapy, with requisite follow-up over many years," Stainback told Heartwire. "When a dramatic plaque burden is demonstrated, it seems to make sense that doctors and patients may take this more seriously than the theoretical risk. The somewhat-contentious remaining issue is that asymptomatic at-risk patients would presumably already have aggressive prevention measures in place, regardless of these additional imaging studies."
Dr. Lincoln Berland, vice chairman for quality improvement and patient safety at the University of Alabama at Birmingham, told AuntMinnie.com that, while he did not specialize in cardiac imaging, general caveats about the risks of screening too many individuals are certainly applicable to the new law.
"Cardiac disease kills more people than anything else in the U.S., so naturally there is great interest in trying to decrease cardiac deaths," Berland wrote in an e-mail to AuntMinnie.com. "One problem with screening that is particularly troublesome here is the huge numbers of people who would be candidates for scanning. Usually, scanning only becomes cost-effective when at least a moderate-risk population is selected."
Incidental findings are quite common in any screening program, leading "to a substantial number of extra tests, primarily for what turns out to be benign disease," he added. "This is one of the factors that makes screening less cost-effective," Berland stated.
The relationship between better healthcare and cost is widely misunderstood, Berland wrote. While screening may save lives by increasing quality-adjusted life years (QALY), the effort is almost always accompanied by higher costs. In the new law, these costs are likely to be significant because of the large number of people who are candidates. Preventive strategies such as diet and medication may or may not increase costs.
"The Texas law mandating [screening] is bold, but it may prove expensive, with an uncertain effect on outcomes, Berland wrote. "Hopefully, if this is implemented, it can be scientifically studied to help answer the important questions about its cost-effectiveness."
By Eric Barnes
AuntMinnie.com staff writer
August 17 2009
Related Reading
Heart groups update cardiac radionuclide guidelines, June 11, 2009
SCCT publishes cardiac CTA guidelines, May 7, 2009
Framingham risk doesn't predict plaque burden, January 5, 2009
AHA urges cautious use of coronary CTA and MRA, July 9, 2008
ASE unveils new stress echo guidelines, September 7, 2007
Copyright © 2009 AuntMinnie.com