
Virtual colonoscopy is not only faster, it's just as accurate when readers increase the field-of-view and perform a single fly through rather than two for each view (prone and supine), say researchers from the University of Wisconsin in Madison.
Increasing the field-of-view (FOV) angle from 90° to 120° on a standard 3D display enabled the group to halve the number of supine and prone fly-through passes, according to a study in the Journal of Computer Assisted Tomography (July-August 2009, Vol. 33:4, pp. 631-635).
The wider FOV technique not only saves time in virtual colonoscopy (also known as CT colonography or CTC), it "diminishes the need for the more distorting virtual dissection displays ... which are unproven in the screening setting and likely have a more difficult learning curve," wrote Dr. Perry Pickhardt in an e-mail to AuntMinnie.com.
Pickhardt, an associate professor of radiology at the University of Wisconsin, and colleagues Dr. Clark Schumacher and Dr. David Kim performed the retrospective study of 73 patients whose polyps had been detected on virtual colonoscopy with a traditional primary technique (four-way fly through at a 90° FOV) and then confirmed and removed at optical colonoscopy.
All of the primary 3D exams were performed by two experienced radiologists using a 120° FOV on 73 patients harboring 104 colonoscopy-proven polyps 6 mm or larger. Of the 104 polyps, 55 were small (6-9 mm) and 49 were large (> 10 mm), with an average polyp size of 13.3 mm.
Patients underwent a cathartic bowel prep the evening before the exam consisting of sodium phosphate or magnesium citrate solution combined with 2% barium and diatrizoate oral contrast tagging agents.
CO2 colonic distention was performed using an automated insufflation device (ProtoCO2L, Bracco Diagnostics, Princeton, NJ). MDCT (LightSpeed 8- or 16-detector-row scanners, GE Healthcare, Chalfont St. Giles, U.K.) was performed using 1.25-mm collimation, 120 kVp, and modulated low-dose mAs in all cases. The imaging data were sent to a dedicated 3D VC workstation (V3D Colon, Viatronix, Stony Brook, NY) for review.
All 104 (100%) polyps were detected with the single-pass 3D evaluation on either the retrograde supine or antegrade prone fly through, with 86 (82.7%) of 104 polyps seen on both fly-through views, the authors reported.
"Of the 18 polyps detected on only one of the two 3D endoluminal passes (10 prone, eight supine), 13 were either submerged under fluid (n = 12) or within a collapsed segment (n = 1); therefore, these were also undetectable on the corresponding 90° bidirectional fly through," they explained.
The remaining five (4.8%) polyps were located behind a fold, but all of these lesions were detected on the other fly-through pass in the reverse direction.
"In this study, we have demonstrated that increasing the FOV angle on the 3D endoluminal display from 90° to 120° can decrease the total number of fly-through passes without degrading the sensitivity for polyp detection," Pickhardt and colleagues wrote.
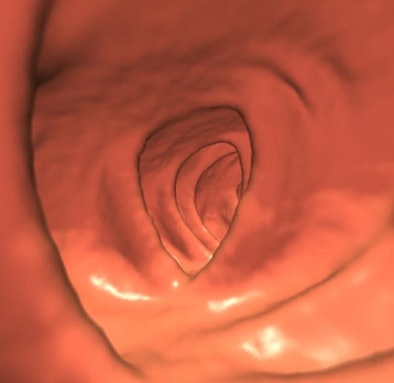 |
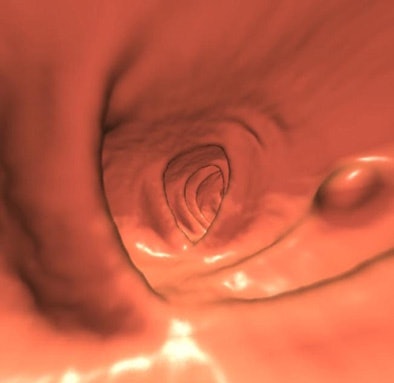
| 7-mm polyp along centerline was not visualized on two-way 90° fly through (above), but was seen on single-pass 120° exam (below). Images courtesy of Dr. Perry Pickhardt. |
 |
Since the study was completed, the group has found polyps that were visible using the wide FOV approach, but were not seen at the two-way fly through at 120° FOV. "This alteration in our interpretive approach may represent a win-win in terms of both polyp detection and reading efficiency," they wrote.
The authors believe that reporting precise interpretation times might have been misleading. However, they noted that typical four-pass 3D interpretations (two prone, two supine) are generally in the five- to 15-minute range, including a combined 3D-2D assessment and extracolonic evaluation. Because the navigational flight speed is the same for 90° and 120° FOV methods, the latter method requiring half as many passes (one each for prone and supine) is associated with "significant time savings," they wrote.
Several different kinds of 3D displays have been developed, and the systems generally present a trade-off between the degree of mucosal visualization and the amount of geometric distortion. For example, while one method may visualize more of the colonic mucosa, potentially reducing interpretation time, it can produce greater visual distortion that impairs lesion detection, Pickhardt and colleagues wrote.
Alternative displays such as virtual dissection and the cube display may be used to supplement standard 2D virtual colonoscopy, but only the 3D fly through has been clinically validated.
"One concern with the nonstandard 3D displays is that a more difficult learning curve could negate any gains related to decreased interpretation time," the group wrote. "Of course, the 2D display remains an essential companion for the ultimate characterization of findings, regardless of the 3D format that one uses."
Fortunately, the gap in performance among different 3D endoscopic visualization systems on the market has narrowed considerably in recent years, they added.
In general clinical practice, "we recommend toggling the FOV angle at 3D endoluminal navigation between and 120° and 90°, with the wider angle used primarily for initial polyp detection and the narrower angle used for undistorted measurement and image capture," they wrote. "In a typical screening case, one-way fly through of both the supine and prone displays with a 120° wide-angle FOV, supplemented by the missed region tool for patches of unseen mucosa (and secondary 2D evaluation), will suffice. For difficult cases with suboptimal distention, however, we generally still perform two-way navigation using the wide-angle setting, which will typically cover 98% to 99% of the evaluable surface."
The study demonstrates that increasing the FOV angle from 90° to 120° on standard 3D endoluminal virtual colonoscopy permits a decrease in the total number of supine and prone fly-through passes from four to two, without impairing overall polyp detection or introducing unacceptable distortion, the authors concluded.
"This results in a facile, time-efficient approach to CTC interpretation that is well suited to a busy clinical practice setting," they wrote. "This diminishes the need for the more distorting virtual dissection displays under investigation, which are unproven in the screening setting and likely have a more difficult learning curve."
By Eric Barnes
AuntMinnie.com staff writer
August 14, 2009
Related Reading
VC CAD plus 3D improves sensitivity for novice readers, April 21, 2009
Virtual colonoscopy beginners do better with 3D data, February 5, 2009
Wider 3D viewing angle may aid polyp detection, September 9, 2008
'Filet view' VC software slices reading time, October 6, 2005
Cubism shapes the art of virtual colonoscopy, October 6, 2003
Copyright © 2009 AuntMinnie.com




















