CHICAGO - Data from a small series of patients suggest that percutaneous ultrasound-guided placement of a partial-breast irradiation (PBI) balloon is a safe and efficient option to whole-breast radiation following lumpectomy for treatment of early-stage breast cancer.
Use of the MammoSite catheter by Cytyc of Marlborough, MA, "allowed a full radiation dose to be delivered in five to seven days versus the six-week regimen used for whole-breast radiation," said Dr. Ellen Mendelson, the director of breast imaging at Northwestern University's Feinberg School of Medicine in Chicago.
Mendelson reported the results Wednesday at the 2006 RSNA meeting.
But Mendelson cautioned, "this catheter really should only be percutaneously placed by radiologists because we are the only physicians who fully understand the geometry of ultrasound that is required for safe placement and radiation dosing."
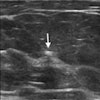
The safety issue, she said, involves the need for adequate thickness between the seroma and the skin. "This needs to be carefully measured and a thickness of 0.6 cm or more is required," she said.
Moreover, the catheter is introduced to the seroma along a trocar-created tract, "which again requires very careful ultrasound guidance."
Mendelson said the MammoSite catheter is one of several PBI techniques being tested in an ongoing 3,000-patient trial that will compare whole-breast radiation to PBI.
In her series, women with tumors smaller than 2.5 cm (stages 0, I, and II) with negative margins and negative lymph nodes following lumpectomy, and who had a skin-to-seroma thickness of 0.6 cm or more, were eligible for PBI.
Among 75 women assessed for PBI from May 2002 to April 2006, 44 women met the entry criteria. "Most of the women who failed to meet the criteria did so because the tissue thickness between seroma and skin was less than 0.6 cm," she said.
Inserted using topical anesthesia, the catheter was filled with 5 mL of nonionic contrast agent and up to 60 mL of saline -- enough to fill the entire cavity.
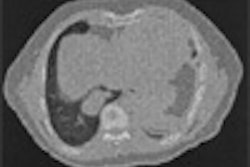
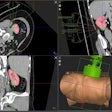
The patients were then sent to radiation oncology for a second measuring of the thickness between the seroma and the skin, as well as CT-based dosimetry to determine the dwell position of high-dose rate iridium-192 sources. Over the next five to seven days, 10 fractions with twice-per-day (3.4 Gy) brachytherapy were delivered.
Nine of the 46 eligible women agreed to PBI and 34 successfully completed treatment. One woman who was considered eligible at first measurement was found to be ineligible when the skin-to-seroma thickness was discovered to be too thin at the second measurement.
No complications occurred during the catheter placements or removals, but one catheter ruptured during treatment and required replacement.
By M. Mary Conroy
AuntMinnie.com contributing writer
November 30, 2006
Related Reading
Breast brachytherapy shows good results, October 19, 2005
Breast tumor surgical margin, histology should guide MammoSite use, September 13, 2005
Good short-term outcomes achieved with accelerated partial breast irradiation, September 2, 2005
Breast MR helps refine partial-breast irradiation, October 19, 2005
Balloon cath brachytherapy offers local breast cancer control, better cosmetics, March 30, 2005
Copyright © 2006 AuntMinnie.com