MR-guided interstitial brachytherapy for recurrent endometrial cancer prevents inadvertent radiation doses to the bladder and rectum. In addition, MRI guidance allows for conformal treatment planning and accurate tumor delineation, according to a Boston-based radiation oncologist.
Dr. Akila Viswanathan said she decided to try this technique after she found established methods lacking. Viswanathan is from Brigham and Women's Hospital and the Dana-Farber Cancer Institute.
"When I started doing interstitial treatment, and did CT simulation, I was pretty surprised to see that there would be needles inserted into the bladder and rectum," said Viswanathan in a presentation at the 2005 American Brachytherapy Society (ABS) meeting in San Francisco. "We would not load these (brachytherapy) catheters, but I was concerned that this was occurring. Had I not had my CT simulation, I may have loaded these cases inadvertently."
For this research, 10 patients (median age 61 years) were enrolled between February 2004 and April 2005. There were eight cases of endometrioid adenocarcinoma, one case of papillary serous carcinoma, and one case of carcinosarcoma. The median tumor size on MR was 4.86 cm. Eight patients received external beam radiation therapy (EBRT) immediately before brachytherapy; two patients had EBRT six months in advance.
Scanning was done on a 0.5-tesla MR therapy unit. T1-weighted and T2-weighted images were acquired. The patients had epidurals and were under general anesthesia. The foley balloon was inserted followed by the obturator and the template, which was sutured in four corners. A median number of 12.9 interstitial catheters were placed.
"We then have the radiologist look at the series of MR images obtained and reposition the obturator so that the needles were directed at the tumor," Viswanathan explained. "We then do the insertion on real-time MR guidance. It doesn't mean that as we are putting in the needles, we are seeing them go in. It does mean that we put the needles in, scan the patient in ... axial or sagittal planes, look at where the needle is, and readjust. Then we get final MR imaging after all the needles have been inserted and we're happy with our tumor volume."
 |
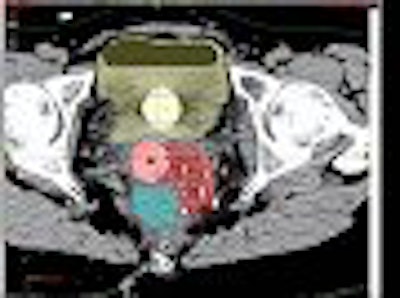
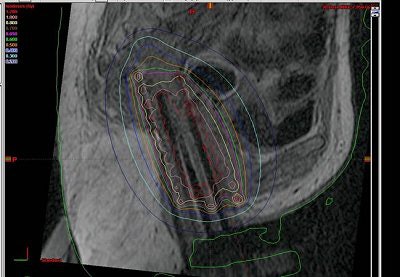
| No inadvertent insertion of interstitial catheter into bladder or rectum noted on CT (below) after MR (above). |
 |
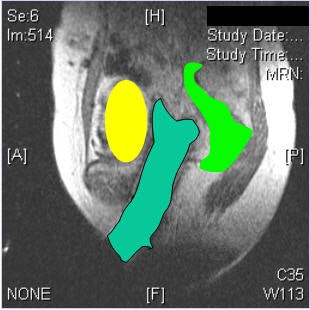
The patients' legs were then brought down and they were reimaged for the CT simulation. "We learned that it was very important to image with the legs down. There was substantial movement with the legs down. But once we figured that out, we were able to perfectly reconstruct the images so that the catheters lined up on MR," Viswanathan said.
Patient follow-up was done at 14, 90, and 180 days postprocedure "The end points of the study were whether or not there was an insertion into the bladder or rectum; whether or not we were able to accurately reconstruct the interstitial implant on MR; what the tumor volume (CT versus MRI) was; the calculated dose-volume histogram (DVH) for the bladder, rectum, and target tissues; and also to assess our normal tissue toxicity," she said.
The results showed that protection of the bladder and rectum was achieved. In all 10 cases, there was no inadvertent insertion.
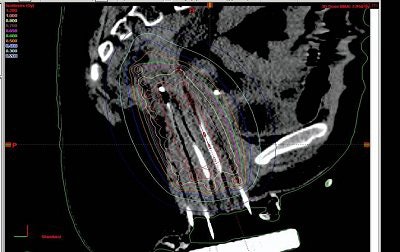 |
| Interstitial reconstruction, MR (above) versus CT (below). Patient must be imaged with legs down. |
 |
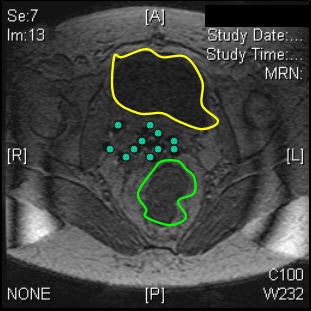
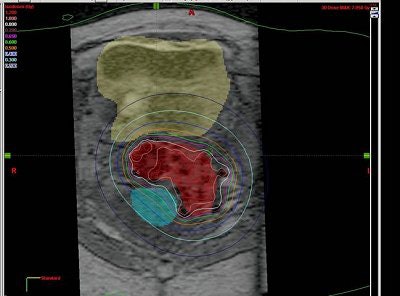
Based on the DVH analysis -- done with CT volumes because that is the standard, Viswanathan added -- the median tumor volume was 80 cc. The median V150 was 60%, the median V90 was 82%, and the median V95 was 90%.
"For bladder and rectal DVHs, we saw that the median bladder total volume was 68 cc. We then calculated the 2-cc and 5-cc percent-of-treatment to the bladder volume and it was 80% and 70%, respectively," she said. "The median rectal volume was contoured for 55 cc and we saw that the 2-cc and 5-cc volumes were 90% and 80% of our prescription."
During the follow-up period, there were two cases of grade 1 skin toxicity and rectal toxicity (diarrhea). At the time of ABS presentation, there were no reported cases of proctitis, Viswanathan said.
"We concluded that MR-guided interstitial brachytherapy is feasible. It does prevent the insertion into the bladder and rectum. It does allow conformal treatment planning and accurate delineation of the tumor, bladder, and rectum," she stated.
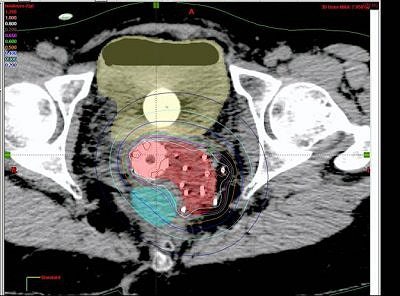 |
| Tumor volume on MRI (above) and CT (below). Images courtesy of Dr. Akila Viswanathan. |
 |
However, Viswanathan pointed out that this was not a study on survival statistics, but on whether MR-guided interstitial brachytherapy was possible. She added that the radiation doses to the rectum were higher than her group would have liked and urged other practitioners to be cognizant of this when providing interstitial brachytherapy in these patients.
Viswanathan told AuntMinnie.com that her group will continue to test MRI-guided brachytherapy in a larger group of patients. The team also plans to do a cost analysis of MRI versus other imaging modalities.
By Shalmali Pal
AuntMinnie.com staff writer
July 5, 2005
Related Reading
Raloxifene may protect against endometrial cancer, May 17, 2005
Endometrial cancer more aggressive in African-American women, March 23, 2005
Copyright © 2005 AuntMinnie.com