Virtual colonoscopy screening isn't ready for population-wide screening in the U.S. just yet, Dr. Abraham Dachman told a group of radiologists in June. But the deficiency has more to do with dollars, documentation, and training capacity than the exam itself.
Much work remains before virtual colonoscopy can screen the large numbers of patients who will need colorectal exams, said Dachman, who is a professor of radiology and director of computed tomography at the University of Chicago in Illinois.
First, if VC is to succeed as a testing option, providers must be reimbursed for their exams, Dachman said at the 2005 International Symposium for Multidetector-Row CT in San Francisco. "If we can't make money doing the procedure, it's not going to take hold," he said.
Ironically, the new category III CPT data-gathering codes introduced in 2004, lauded as the next step in bringing VC to the mainstream, had the effect of stopping reimbursement for some VC studies that were previously billed and reimbursed as noninfused abdomen exams, taking reimbursement a step backward, Dachman said.
And thanks to virtual colonoscopy's steep training curve, accurate and cost-effective reading methods, including CAD, and novel viewing methods under development will be needed to help nonexperts interpret the exams.
More training opportunities will be needed to handle more providers, Dachman said. "Courses, books, Web-based datasets, and self-teaching modules are now available, but I don't think we can accommodate everybody with what we have on board right now, if everybody wanted it right away."
More studies, cost-effectiveness models
Another large prospective trial will be needed to confirm the excellent results that Dr. Pickhardt and colleagues achieved in their multicenter trial two years ago (New England Journal of Medicine, December 4, 2003, Vol. 349:23, pp. 2191-2200).
A new megastudy is in the works, of course. The National CT Colonography Trial (ACRIN protocol 6664) began in February, though results won't be available for several years. Even if it demonstrates high accuracy for VC, models will still need to demonstrate that screening is cost-effective, Dachman said.
"I personally think there are models that show that it does pay, if we really look at average-risk patients, and we're really increasing the number of patients who have optical colonoscopy who really need it," he said.
Finally, virtual colonoscopy must be compared to technologies that may someday compete with it, such as DNA stool testing and other emerging techniques.
A good start
How has VC gotten this far? There are several good reasons, according to Dachman. First, people know that colorectal cancer screening is effective. Second, national compliance with traditional screening methods is unacceptably low. And third, optical colonoscopy is expensive and hard to get.
"We're doing a much better job as a nation letting people know that they need to screen with mammography compared to colorectal cancer -- even though colorectal cancer is the second most common cause of cancer deaths when you combine men and women, and the most common cause of cancer deaths in nonsmokers," Dachman said. "And unlike mammo, you're not just looking for an early cancer because of the adenoma carcinoma sequence -- you're looking for adenomas. So (colorectal cancer screening) is a great model, and we're doing a very poor job."
Just 44% of the over-50 U.S. population has ever had conventional colonoscopy or flexible sigmoidoscopy, according to the U.S. Center for Disease Control and Prevention's state-based Risk Factor Surveillance System, 1999. Conversely, 82% of women age 40 and older have had a mammogram.
Still, the waiting lists for optical colonoscopy are long, Dachman said, and some are tired of waiting for their exams. "I started offering VC for nonresearch purposes about five years ago because I got tired of saying no to patients who were calling," Dachman said.
Widespread VC screening in the U.S. will ultimately rely on funding that must be approved by the U.S. Congress in the form of a national coverage decision that authorizes screening virtual colonoscopy (CT colonography) as a covered colorectal screening exam.
Even without the national coverage decision VC proponents have been looking for, however, progress can and does happen at the local level, Dachman said, citing the success of a screening program initiated by Dr. Perry Pickhardt from the University of Wisconsin in Madison.
Medicare movement
Last year, Pickhardt's team convinced the Physicians Plus Insurance Company in Madison, WI, and other payors to begin reimbursing screening virtual colonoscopy in both symptomatic and asymptomatic patients. Approximately 4% to 5% of these VC screening patients are referred for same-day optical colonoscopy, Dachman said.
As of this week, the Wisconsin group has performed close to 2,000 VC exams, now at the rate of about 40 per week, Pickhardt told AuntMinnie.com.
And last month the local Medicare provider approved payment of diagnostic virtual colonoscopy in five Midwestern states, an important incremental improvement in the reimbursement picture.
The local Part B Medicare decision was especially welcome news for Midwestern providers, inasmuch as it restored reimbursement for diagnostic VC exams that had once been reimbursed by Medicare and other payors as diagnostic abdominal studies, but were no longer reimbursed after the introduction of category III CPT codes (0066T for screening VC and 0067T for diagnostic VC) in 2004. The new codes became the Medicare standard in January 2005.
Another major step has been the development of reporting standards by a group of VC researchers, Dachman noted. A final version was published two months ago (Radiology, July 2005, Vol. 236:1, pp. 3-9).
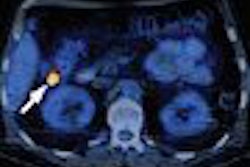
As for the exam itself, CAD represents the next major step toward improving reader confidence, Dachman said. Novel viewing systems, also under development, will improve VC interpretation, paving the way to mass screening and reduced variability in reading performance.
"Many of these novel viewing systems allow the possibility of increasing speed or increasing accuracy," he said, adding that more research is needed to determine the learning curve and optimize learning methods.
The ability to detect and characterize flat lesions, which are generally easier to see in optical colonoscopy than VC, will be another major issue related to improving interpretation methods. And the 2D versus 3D debate isn't over yet, he said.
"I personally think that (both) 2D and 3D (interpretation) is needed on everybody, and I think we need to look at flat lesions for everybody, or else we'll be handing this technology over to the gastroenterologists," Dachman said.
Still, there is good news about flat polyps in a retrospective examination of data from the National Polyp Study, which showed that flat lesions are not associated with an increased risk of high-grade dysplasia. The risk is size-dependent, as in other lesions, Dachman said (Clinical Gastroenterology and Hepatology, October 2004, Vol. 2:10, pp. 905-911).
A better prep
Prep is a big issue as well -- patients have responded clearly in surveys that they want it to be more comfortable and less painful. Their needs have been addressed somewhat in the development of new exam techniques, smaller catheters, and bowel insufflation with CO2 rather than room air.
This is a positive development, because patients' experience with virtual colonoscopy will have a big impact on how willing they are to return for rescreening -- and as a result, the extent to which VC screening will truly be cost-effective, Dachman said.
Fortunately, prepless VC exam is feasible and potentially accurate, as recently demonstrated by Iannaccone and colleagues in Rome, who achieved per-patient sensitivity of 86% for polyps 6 mm and larger, and 95.5% for polyps 8 mm and larger, with a prepless exam in 203 patients (Gastroenterology, November 2004, Vol. 127:5, pp. 1,300-1,311).
Still, "the devil is in the details," Dachman said. "They used a large volume of (contrast agent) gastrografin, which may have a cathartic (and therefore cleansing) effect."
The case for the VC screening model remains solid, he said. Small lesions, particularly those 5 mm and smaller, probably don't grow very rapidly and may even regress in size, according to a study of diminutive polyps followed up annually by optical colonoscopy (Scandinavian Journal of Gastroenterology, September 1986, Vol. 21:7, pp. 853-862).
Even now VC is the best option for patients who either have an incomplete colonoscopy or cannot undergo colonoscopy, Dachman said.
"Why is it not ready for mass screening? I think it's primarily not ready because it's going to be hard for us to train everybody, there is a long learning curve, and training opportunities are limited," he said.
Dachman said that interest in training actually declined somewhat last year, as reimbursement for diagnostic CT colonography was curtailed. Fortunately, the local coverage decision in the Midwest has changed the reimbursement picture for the better, he said, and other regions can potentially benefit as well.
"Local lobbying will help -- not only with Medicare, but pressure on local insurance to follow that model," Dachman said." Dedicated software will help make VC more practical for mass screening. And certainly the results of the ACRIN trial, which we're going to have to wait a while for, will be really critical in Medicare's decision, and maybe Congress' decision on the national level."
By Eric Barnes
AuntMinnie.com staff writer
September 23, 2005
Related Reading
Virtual colonoscopy: Ready already for those who know how, April 15, 2005
CMS approves VC after failed colonoscopy in Midwest, August 30, 2005
VC practice thrives in Wisconsin, May 10, 2005
Debate over 2D versus 3D VC reveals subtle differences, January 21, 2005
VC gets long-awaited reporting standards, November 2, 2004
Copyright © 2005 AuntMinnie.com