Two computer-aided detection (CAD) systems yielded varying sensitivity in detecting small invasive breast carcinoma, according to research published in the October issue of Radiology.
"A statistically significant difference was observed in per-study and per-image sensitivity in our mammography dataset with small (< 16 mm), noncalcified invasive breast malignancies between two CAD systems," wrote a research team led by Dr. Richard Ellis of Gunderson Lutheran Health System in La Crosse, WI. "Differences in per-study specificity and mass false marker rate were noted but were not statistically significant.
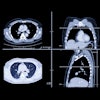
To retrospectively compare two CAD systems for detecting invasive breast cancers manifesting as noncalcified masses smaller than 16 mm, the study team collected 192 consecutive mammograms from two institutions. Of the mammograms, 182 were unifocal, six were multifocal, and four were bilateral cancers (Radiology, October 2007, Vol. 245:1, pp. 88-94).
The studies were then evaluated using version 5.0A of R2's ImageChecker M1000 software (Hologic, Bedford, MA), and version 6.0 (using midoperating point) of SecondLook software (iCAD, Nashua, NH). Masses were characterized using the Breast Imaging Reporting and Data System (BI-RADS).
The researchers then determined per-study specificity and mass false marker rate by using 51 normal four-view studies, while only scoring the mass false-positive marks for noncalcified masses.
The chart below shows the results for both CAD systems for per-study sensitivity, per-image sensitivity, per-study specificity, and mass false-positive (FP) marker rate.
|
The researchers determined that the ImageChecker software had significantly better overall per-study and per-image sensitivities (p < 0.001), and had a nonsignificant higher per-study specificity and lower mass false marker rate on normal studies. In addition, they found that CAD results revealed at least a 20% variation between BI-RADS categories 4a and 5 for per-study and per-image sensitivities.
"Our results suggest that for the CAD systems evaluated, there is a need for continued improvement in detection of invasive breast carcinomas smaller than 16 mm, especially for those in BI-RADS category 4a or 4b, to achieve the authors' desired goals for a study sensitivity 90% or higher, image sensitivity 70% or higher, study specificity 50% or higher, and a false marker rate 1 or lower," the authors wrote.
The researchers noted the importance of appropriate orientation and training for a new CAD system into a screening mammography program.
"It should be incumbent on each institution that uses CAD to determine the value of its system for cancer rate detection, primary prognostic variables for the detected cancers, recall rates, and financial implications both before and after the installation of CAD," the authors noted. "Given the variable performance among radiologists in the interpretation of a screening mammogram, the value of CAD will also vary."
By Erik L. Ridley
AuntMinnie.com staff writer
October 5, 2007
Related Reading
Breast CAD results vary based on mammography view, August 6, 2007
CAD still not out of the woods, despite Oregon payor's reversal, July 24, 2007
Oregon payor reverses stand, reinstates CAD payments, July 23, 2007
NEJM study prompts Oregon payor to cancel CAD reimbursement, July 11, 2007
Studies show CAD matches up well with CR mammo, FFDM, May 24, 2007
Copyright © 2007 AuntMinnie.com