Dr. Robin Wilson recently moved from the Nottingham Breast Institute in Nottingham, U.K., to London-based Guy's Hospital and he noticed more than just a change in scenery.
"There's a variety of practice around the world as to how you deal with male breast cancer and how you investigate male breast cancer," Wilson said during a talk at the recent 2007 Breast Course in Key Largo, FL. "(I) spent 18 years in (Nottingham) where we never did a single male mammogram and moved to (Guy's) where every man who comes through the door seems to have a mammogram."
Wilson was no doubt engaging in a little hyperbole, but the incidence of this rare disease (less than 1% of all breast cancers worldwide) has shifted in recent years, he noted. In the last 20 years, the incidence of breast cancer among U.S. males has gone up 25%, he said. Of course, one main reason for this is that people are living longer and breast cancer is an older person's disease, he added.
But diet, genetics, and environment also play a role in male breast cancer, a disease which generally peaks at age 71 for men (versus 72 and 75 for women) and, unfortunately, is diagnosed at an advanced stage (stage III or IV), leading to increased mortality.
Of course, routine screening for male breast cancer simply isn't done -- and with good reason given how uncommon the disease is. Nonetheless, imaging experts should be aware of when to perform mammogram or breast ultrasound exams on male patients and what to look for on these exams, Wilson said.
"I'm a great believer in working out what added value any particular test has because if it doesn't have any added value, there's no need to do it," he said.
Course of male breast cancer
As Wilson mentioned, certain risk factors can predispose a man to breast cancer:
- BRCA2 genetic mutation
- Environment, such as high-fat diet, excessive alcohol consumption, and exposure to high ambient temperatures or exhaust fumes
- Other disease states that increase estrogen levels
- Testicular damage
- Liver disease
- Chest radiotherapy
The majority of male breast cancer (93%) is invasive ductal carcinoma. Lobular carcinoma is five times less common in men than in women, Wilson said. Still, treatment regimens are similar to those used for female breast cancer, although breast-conserving surgery is unnecessary. Most men automatically have a mastectomy. Also, because the vast majority of male breast cancer is estrogen receptor-positive/HER2-negative, hormone adjuvant therapy is standard after surgery, he stated.
Clinical presentation
"The vast majority of men who appear at your clinic (for breast imaging) have gynecomastia or pseudogynecomastia," Wilson noted. "The difference is that gynecomastia is due to the development of breast tissue, while pseudogynecomastia is just fat (and) being overweight."
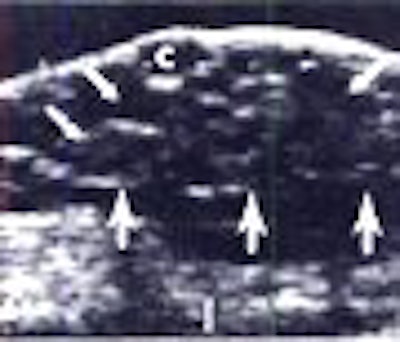
But if the patient is actually sent for imaging, it's because the referring physician has a strong suspicion of breast cancer. Making the differential diagnosis between gynecomastia and breast cancer is fairly simple, he said. Gynecomastia is nodular and dendritic, and is easy to identify on ultrasound.
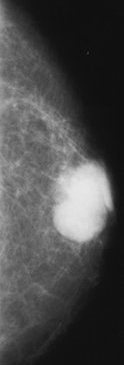
 |
| Above, 32-year-old man undergoing treatment for brain tumor complained of soreness in the left breast. A sagittal sonogram through left areolar region. Expanding focal hypoechoic area (arrows) in subareolar area secondary to focal gynecomastia. Below, 59-year-old man who underwent modified left radical mastectomy for adenocarcinoma of the breast. A sagittal sonogram of right breast shows sebacious cyst and early changes of diffuse gynecomastia. Wigley KD, Thomas JL, Bernardino ME, Rosenbaum JL, "Sonography of gynecomastia" (AJR 1981; 136:927-930). |
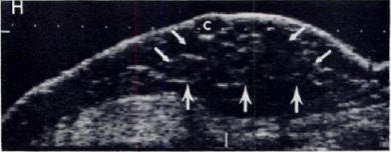 |
In fact, Wilson said he preferred ultrasound to mammography when evaluating the male breast. "To my mind, ultrasound is the imaging technique of first choice if clinical assessment is equivocal. Mammography very rarely adds anything to the diagnostic process," he said. "An ill-defined, retroareolar mass is the commonest clinical radio finding by far."
Wilson told AuntMinnie.com that he recommends using a small (5-cm) probe of 10-15 MHz to visualize male breast tissue behind the nipple. He also suggested using lots of gel and angling the probe behind the nipple.
In 75% of the cases, men present with a painless breast, and nipple involvement (change or retraction) is quite common, Wilson said. A recent paper on gynecomastia management stated that the condition is present in 30% to 50% of healthy men (International Journal of Clinical Practice, March 16, 2007).
The presence of a firm, palpable mass is generally indicative of gynecomastia or pseudogynecomastia, and there is no need for imaging, Wilson said. Using needle biopsy, the referring clinician should be able to make the final diagnosis.
If biopsy results show malignant cells, then the patient should undergo ultrasound of the axilla as part of pretreatment staging, as it is most likely that the lymph nodes are involved, Wilson said. If ultrasound results are normal, yet the patient presented with unilateral single-duct discharge, then Wilson recommends turning to mammography.
Why ultrasound?
A Breast Course attendee asked Wilson why he preferred sonography over mammography in male patients. Wilson said he found it easier to make the differential diagnosis sonographically, and that the exam was less expensive. In addition, male patients said they found it more comfortable.
A recent study out of the Mayo Clinic in Jacksonville, FL, determined that mammography added "little information" in male breast cancer patients, adding that the modality may be of benefit only for guiding biopsy (Mayo Clinic Proceedings, March 2007, Vol. 82:3, pp. 297-300).
However, Wilson acknowledged that billing differences between the U.S. and the U.K. health system -- where reimbursement is not broken down by modality -- may make mammography the more practical choice.
 |
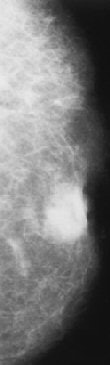 |
| Infiltrating ductal carcinoma. Above left, craniocaudal mammogram shows a lobulated mass with a primarily well-defined margin and eccentrically located relative to the nipple. Above right, craniocaudal mammogram shows a retroareolar mass with ill-defined margins and nipple retraction. Figure 8,9. Appelbaum AH, Evans GFF, MB, Levy KR, Amirkhan RH, Schumpert TD, "Mammographic Appearances of Male Breast Disease." RadioGraphics. 1999;19(3):559-568. | |
In answer to another question about fibroadenomas in the male breast, Wilson said he could not find any published work on the subject, but that it wasn't likely to be a problem in men.
"The peak age of (fibroadenoma) incidence is 18-30, and the male breast is not being subjected to the same hormonal influences (as women)," he explained.
Dr. Steve Harms, from the University of Arkansas for Medical Sciences in Little Rock, asked Wilson for his thoughts on regularly screening men who carried the BRCA2 mutation.
"If they are BRCA2-positive, I'm not sure that you would do mammography routinely or even MR," Wilson replied. "We would recommend that they are diligent about self-breast exam."
Wilson also directed his audience to the most current and comprehensive papers on the subject:
- "Male breast cancer," Lancet, February 18, 2006, Vol. 367:9510, pp. 595-604
- "Breast carcinoma in men: A population-based study," Cancer, July 2004, Vol. 101:1, pp. 51-57
- "Mammographic Appearances of Male Breast Disease," RadioGraphics, May-June 1999, Vol. 19:3, pp. 559-568
By Shalmali Pal
AuntMinnie.com staff writer
April 4, 2007
Related Reading
Male mammograms: Positioning tips to ensure image quality, August 18, 2005
Tamoxifen can reduce breast pain in prostate cancer patients, April 14, 2005
Breast cancer on rise in men, study shows, May 25, 2004
Mammography is tops for breast cancer detection -- in men, May 3, 2004
Copyright © 2007 AuntMinnie.com