Advanced breast ultrasound applications offer valuable information on lesion elasticity and fluidity, helping clinicians differentiate between masses and cysts, as well as benign and malignant lesions. In two recent studies, U.S. radiologists used streaming detection to further evaluate indeterminate sonographic breast masses, while a group from Japan explored the diagnostic application of ultrasound elastography.
Streaming for cysts
On ultrasound, simple cysts are aptly named with their easily identifiable traits -- they are anechoic, well-circumscribed masses with imperceptible walls and posterior acoustic enhancement. Solid masses, on the other hand, present a diagnostic conundrum as their features can overlap with those of cysts. The designation of a simple cyst versus a complicated cyst versus a solid mass can determine whether the patient should undergo aspiration or follow-up imaging, according to Dr. Mary Scott Soo and colleagues from Duke University in Durham, NC.
Soo's group and Siemens Medical Solutions tested streaming sonography for separating cysts from solid masses. "Streaming detection is a novel ultrasonic method that uses acoustic energy to induce fluid flow or acoustic streaming in cyst fluid, which can then be detected with Doppler methods," they explained (American Journal of Roentgenology, May 2006, Vol. 186:5, pp. 1335-1341).
Over a six-month period, this prospective study investigated 39 lesions from 34 patients: 11 simple cysts and seven solid masses in the control group and 21 indeterminate masses.
The streaming detection software was downloaded onto two ultrasound units (Sonoline Elegra, Siemens Medical Solutions, Malvern, PA) and included combined B-mode image, color and spectral Doppler modes with a Doppler tracing function, and an adjustable gate. The entire imaging exam took about five minutes for eight acquisitions. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were assessed.
According to the results, simple cysts in the control group had a mean size of 16 mm and a mean depth of 13.4 mm. Solid masses had a mean size of 7.4 mm and a mean depth of 9.7 mm. Seven simple cysts underwent aspiration to complete resolution. Core biopsies of seven solid masses revealed one malignant lesion.
"Streaming detection was positive for fluid movement and correctly identified nine (82%) of 11 simple cysts," the group wrote, for a sensitivity of 82%, PPV of 100%, specificity of 100%, and NPV of 78%.
For indeterminate masses, the mean size was 10.8 mm and the mean depth was 16.3 mm. Eighteen lesions were aspirated to complete resolution and one was determined to be a solid mass. All lesions were benign with 95% designated as cysts with a mean viscosity of 2.3.
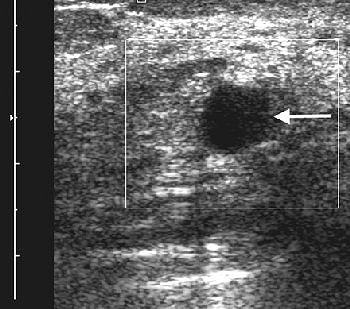 |
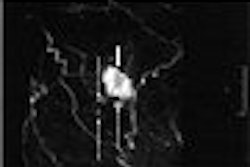
| A 47-year-old woman with palpable mass in left breast considered indeterminate and likely complicated cyst on conventional B-mode sonography. Sonogram of left breast shows 1-cm complicated cyst (arrow) with low-level internal echoes. |
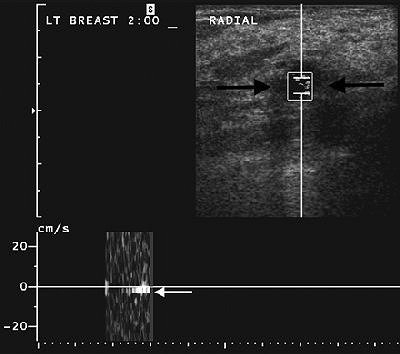 |
| Same patient as above. After one acquisition, streaming detection sonogram shows same cyst with Doppler cursor positioned over cyst (black arrows). Resulting Doppler wave signal shows acoustic streaming seen as white band below baseline (white arrow), indicating fluid-filled lesion. Lesion was confirmed as cyst at aspiration. Soo MS, Ghate SV, Baker JA, Rosen EL, Walsh R, Warwick BN, Ramachandran AR, Nightingale KR, "Streaming Detection for Evaluation of Indeterminate Sonographic Breast Masses: A Pilot Study" (AJR 2006; 186:1335-1341). |
Streaming detection was positive for fluid movement during at least one acquisition, producing a sensitivity of 50% and PPV of 100% for cysts.
"In our pilot study, streaming detection successfully detected acoustic streaming within fluid-filled cysts in half of the indeterminate lesions recommended for cyst aspirations and showed no false-negative results in evaluating solid lesions," the authors stated. "This technique has the potential to be used as a clinical tool to complement conventional breast sonography."
The authors cautioned that streaming detection was not suitable for evaluating complex masses because the detection of cyst fluid would not alter management. They also did not recommend the technique for masses with malignancy markers, such as irregular shape, spiculated margins, and ill-defined margins.
They concluded that streaming detection was a quick way for a radiologist to confirm that an indeterminate lesion was actually a fluid-filled cyst, adding that the streaming software was easily mated with a conventional ultrasound system.
US elastography
Recent studies have reported the success of elastography for evaluating hepatic fibrosis in HIV and cirrhosis in chronic liver disease. Now, Japanese researchers are stating that ultrasound elastography can be used to distinguish benign from malignant breast lesions. Their particular spin on this technique involves a unique tissue strain measurement that they call the combined autocorrelation method (CAM).
"The principle of elastography is that tissue compression produces (displacement) within the tissue.... The CAM method enables rapid and accurate detection of longitudinal displacement by using phase-domain processing without aliasing," explained Dr. Ako Itoh and colleagues at the University of Tsukuba in Tsukuba, Japan, and Hitachi Medical in Kashiwa City, Japan (Radiology, May 2006, Vol. 239:2, pp. 341-350).
For this research, the group performed real-time freehand US elastography in 135 women with 76 benign lesions and 56 malignant lesions. Lesions that were classified as malignant included ductal carcinoma in situ (DCIS) and invasive ductal carcinoma of nonscirrhous type. Benign lesions included intraductal papilloma and fibroadenoma.
All elasticity images were generated with a digital ultrasound scanner and a 7.5-MHz linear transducer (EUB-6500, EUP-L53, Hitachi Medical Systems, Tokyo). "To obtain images that were appropriate for analysis, we applied the probe with only light pressure, which we defined as a level of pressure that maintained contact with the skin and permitted imaging conditions for which the association between pressure and strain were essentially proportional," the authors wrote.
The region of interest (ROI) on elasticity images was drawn to include subcutaneous fat at the top and pectoral muscle at the bottom. Lateral boundaries were set more than 5 mm from the lesion's boundary. Under CAM, each pixel of the elasticity image was assigned one of 256 colors with red representing the greatest strain, blue the least amount of strain, and green the average in the ROI. The color patterns were then scored from 1-5, with the latter indication no strain in the entire hypoechoic lesion.
The final pathologic diagnosis was 59 benign lesions, according to the results. The group found that the mean elasticity score was significantly higher for malignant lesions (4.2) than for benign ones (2.1). Of the malignant lesions, 86% had a CAM score of 4 or 5. Of the benign lesions, 68% had a CAM score of 1 or 2.
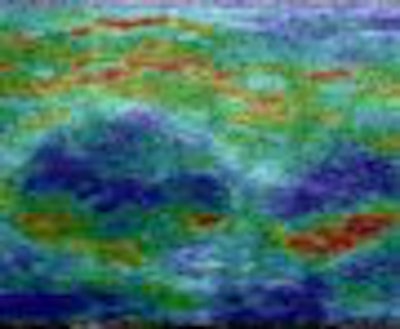
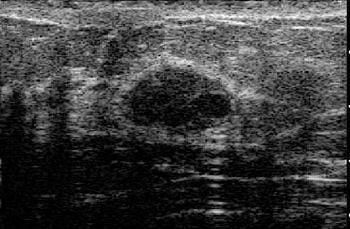 |
| Fibroadenoma with elasticity score of 2 in 39-year-old woman. US images were obtained in transverse plane. Left: On conventional B-mode image, lesion was classified as BI-RADS category 3. |
The area under the receiver operation characteristics (ROC) curve for elastography was 0.9185 versus 0.9153 for traditional ultrasound.
Elastography's sensitivity was 86.5%, specificity was 89.8%, and accuracy was 88.3%. For conventional ultrasound, the sensitivity was 71.2%, specificity was 96.6%, and accuracy was 84.7%.
"The specificity of elastography was not inferior to (i.e., not more than 15% different than) and the accuracy was equivalent to (i.e., within 13% of) that of conventional US," the authors stated.
They highlighted some of the advantages of US elastography with CAM: It was a simple system that provided a higher frame rate while maintaining high image quality. It also allowed for more rapid longitudinal displacement, as well as more robust lateral movement of the probe.
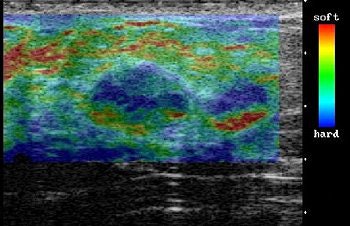 |
| On elasticity image, hypoechoic lesion shows mosaic pattern of green and blue. Figure 3. Ako Itoh A, Ueno E, Tohno E, et al, "Breast Disease: Clinical Application of US Elastography for Diagnosis" (Radiology 2006;239:341-350). |
However, they did note some limitations to this research: Their study population was biased toward cancer patients because they are a referral center. Also, the lesions assessed were predominantly larger ones. Finally, the main pitfall of elastography was that image and the scoring system were influenced by tissue compression. The authors emphasized that it takes practice to apply the right amount of pressure to the breast.
Nonetheless, they predicted that with future improvements, US elastography will become "invaluable" in the clinical setting. "With our system, lesions can be easily found because translucent color scale elasticity images are superimposed on the corresponding B-mode images," they stated. "We believe that, with concomitant use of elastography and conventional US, it may be possible to downgrade some BI-RADS category 3 and 4 lesions to BI-RADS category 2 lesions."
By Shalmali Pal
AuntMinnie.com staff writer
June 16, 2006
Related Reading
Breast surgeon expresses reservations about screening US, May 13, 2006
Expanded role looms for 3D in breast imaging, May 11, 2006
Auto breast US handily spots lesions in early study, January 13, 2006
Compression US plus computer analysis classifies solid breast masses, September 7, 2005
US elastography shows promise as mammography adjunct, March 5, 2005
Copyright © 2006 AuntMinnie.com