Nearly 80% of people who suffer from severe sciatica are never properly diagnosed. The problem is that there is no gold standard for finding the underlying causes of sciatic pain. In fact, most patients have to undergo surgery before a definitive diagnosis can be made. MR neurography could change all that, according to a group of California-based spinal specialists.
"The importance of imaging the sciatic nerve in the evaluation of sciatica of nondisk origin cannot be overemphasized," wrote Dr. Aaron Filler, Ph.D., and colleagues. "This study makes clear that MR imaging without MR neurography is not adequate because the former is unable to diagnose the lesion in many people in whom there are identifiable and treatable abnormalities" (Journal of Neurosurgery: Spine, February 2005, Vol. 2:2, pp. 99-115).
These abnormalities include lumbar disk herniation, piriformis syndrome, and distal foraminal impingements, stated Filler, who is from the Neurography Institute and the Institute for Nerve Medicine in Santa Monica. His co-authors are from Cedars-Sinai Medical Center in Los Angeles and the University of California, Los Angeles (UCLA).
For this study, 239 consecutive patients were assessed either at the Santa Monica facility or at UCLA. If traditional MR failed to assist with a diagnosis, the patients underwent lumbar and pelvic soft-tissue MRI, as well as MR neurography on a 1.5-tesla unit.
Phased-array coils were used to enhance the signal-to-noise ratio. The protocol included T1-weighted spin-echo, FSE, T1-weighted axial, and axial and coronal T2-weighted fat-suppressed imaging. Finally, MRI was performed in nerve-oriented planes, either parallel or perpendicular to the major nerve courses. The images were read by Filler and co-author Dr. J. Pablo Villablanca.
Those who most likely had piriformis syndrome were referred for open-MRI-guided piriformis muscle injection. Others were treated either with fluoroscopically guided spinal injections or MR-guided injections. All patients were followed up from six months to six years.
The results showed that the most common diagnosis was muscle-based piriformis syndrome. MR neurography also proved useful for finding other causes of nondisk sciatica, such as nerve tumors, distal foraminal impingements, and perineural bone fractures.
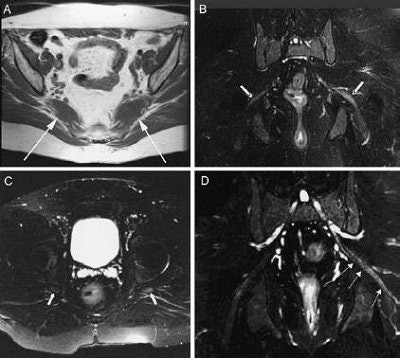 |
| Magnetic resonance neurography findings in piriformis syndrome. A: Axial T1-weighted image of piriformis muscle size asymmetry (arrows indicate piriformis muscles). The left muscle is enlarged. B and C: Coronal and axial images of the pelvis (arrows indicate sciatic nerves). The left nerve exhibited hyperintensity. D: Curved reformatted neurography image demonstrating left sciatic nerve hyperintensity and loss of fascicular detail at the sciatic notch (arrows). Filler AG, Haynes J, Jordan SE, et al, "Sciatica of nondisc origin and piriformis syndrome: Diagnosis by magnetic resonance neurography and interventional magnetic resonance imaging with outcome study of resulting treatment," J Neurosurg Spine 2: 99-115, 2005, Figure 5. |
In particular, the authors praised the modality's ability to depict "exiting spinal roots and nerves, the lumbosacral plexus, and proximal sciatic nerves reliably (identifying) the lesion in most patients in whom routine modalities (lumbar MR imaging and radiography alone) failed to establish a diagnosis."
MR neurography also proved itself in surgical planning by depicting the areas of nerve abnormality, as well as the tissues surrounding the nerves contributing to the disorder.
Successful MR neurography was based on two findings: piriformis muscle asymmetry and unilateral sciatic nerve hyperintensity at the level of the sciatic notch. Together, these criteria gave MR neurography a high specificity of 93% and a moderate sensitivity of 64%.
"Its sensitivity of 64% underscores that either the syndrome produces a relatively low profile of image-based abnormalities or that the imaging method could be improved," the group stated. Still, these MR numbers were an improvement.
"When piriformis muscle asymmetry alone is used as a criterion to identify individuals with piriformis syndrome, the specificity is 66% and the sensitivity is 46%," they pointed out.
Filler's group also found that open-MR guidance allowed for more precise injections in piriformis muscle, nearly eliminating the risk of penetrating the nerve or bowel, and offering better treatment documentation.
They urged physicians to seriously consider adding MR neurography to their diagnostic protocol in patients with sciatica and possible sciatic entrapments.
By Shalmali Pal
AuntMinnie.com staff writer
April 15, 2005
Related Reading
Routine x-rays offer little after lumbar spine fusion, March 22, 2005
MR clarifies paralabral cysts as common source of hip pain, September 6, 2004
Copyright © 2005 AuntMinnie.com