Measurements of soft-plaque volumes calculated on different software platforms following cardiac CT angiography (CCTA) exams can vary widely, according to a study presented this week at the Society of Cardiovascular Computed Tomography (SCCT) meeting in Las Vegas.
Clinicians need to keep these differences in mind when evaluating patients, especially as radiologists learn more about the connection between noncalcified plaque burden and adverse cardiac events, according to researchers from the Medical University of South Carolina (MUSC) in Charleston, who performed the study.
"There is increasing understanding that the noncalcified plaque burden may be even more important than the calcified plaque burden for risk stratification and for patient management, simply because it is the noncalcified plaque burden that is the surrogate for major adverse cardiac events such as unstable angina or sudden cardiac death," said U. Joseph Schoepf, MD, a professor of radiology and medicine at MUSC. The study was presented at the SCCT show by lead author Shane Oberoi.
While calcified plaques tend to cause chronic angina, even more dangerous are sudden cardiac events, which studies have shown are typically caused by the rupture in nonstenotic, lipid-rich noncalcified plaques, Schoepf said. As a result, there is growing interest in improving both the characterization and the quantification of soft plaques on CT.
But unlike calcium volumes, which can be calculated reproducibly on any workstation platform using, for example, the Agatston scoring method, there is no analogous quantification scheme for soft-plaque volumetry; different vendors each have their own proprietary methods of calculating soft plaque.
For the study, Oberoi and Schoepf, along with Christian Thilo, MD, examined 47 patients with documented noncalcified plaque by coronary CT angiography. They recorded patient data including age, sex, race, and body mass index, as well as cardiac risk factors.
Following the administration of beta-blockers, contrast media, and a nitroglycerine tablet, CT angiography images were acquired on a 64-detector-row scanner (Somatom Sensation 64 Cardiac, Siemens Healthcare, Malvern, PA) using retrospective electrocardiogram gating. Images were acquired at a 0.33-sec rotation time, 0.2 pitch, 120 kV tube voltage, and 900 mAs tube current, the authors wrote in an accompanying abstract.
Administration of a test bolus was followed by injection of 50 to 75 mL of a nonionic iodinated contrast agent (350 mgI/mL iohexol, Omnipaque, GE Healthcare, Chalfont St. Giles, U.K.) at 5 mL/sec, followed by a 50-mL saline chaser.
All images were analyzed on three different image analysis platforms:
- Aquarius (TeraRecon, San Mateo, CA)
- Circulation (Siemens)
- Vitrea (Vital Images, Minnetonka, MN)
"These were the ones we could get our hands on, but pretty much every vendor has these noncalcified plaque tools available," Schoepf said. "None of the tools has been validated against an outside gold standard such as intravascular ultrasound, and nobody has looked at whether those tools actually measure the same way," making it impossible to monitor plaque burden over time, he said.
The noncalcified plaque burden was quantified for each patient in each of the three major coronary arteries -- left anterior descending (LAD), left circumflex (LCX), and right coronary (RCA) -- and on each of the three software platforms, set to analyze the entire length of the vessels.
The researchers also generated a centerline through the lumen in each postprocessing software package, and edited the results manually if needed, analyzing the entire vessel.
The trial was performed twice on each platform to gauge reproducibility, Schoepf said. Parameters on the image analysis platforms were modified to quantify the volume of tissue falling between specific attenuation ranges, including 0 to 50 HU for low-attenuation plaque and 50 to 130 HU for medium-attenuation plaque, applied to all workstations.
Although controllable variables were kept constant in all of the analyses, the investigators found considerable systematic differences between the three cardiac image analysis platforms for noncalcified plaque burden software, they said.
After computing the mean, median, and standard deviation of the volume measured by the three software programs, a test of whether there was a trial or temporal effect was made and found to be statistically insignificant (p > 0.05).
Similarly, mean volumes in the three software programs were not different between the two trial time points, showing good reproducibility within each software package, so the results were averaged, Schoepf said.
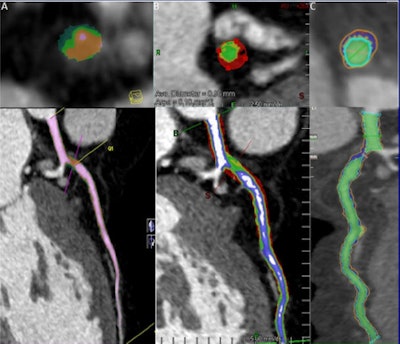 |
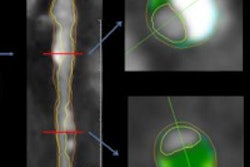
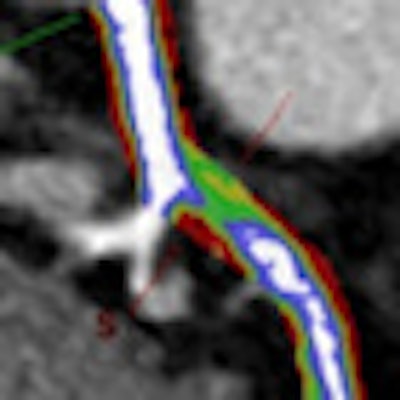
| Automated volumetric measurement of the same noncalcified lesion. (A) Siemens' Circulation: dark green represents < 0 HU, bright green 0 to 50 HU, orange 50 to 130 HU, and pink > 130 HU. (B) TeraRecon's Aquarius: red represents < 0 HU, yellow 0 to 50 HU, green 50 to 130 HU, blue 130 to 350 HU, and white > 350 HU. (C) Vital Images' Vitrea: red represents 0 to 50 HU, blue 50 to 130 HU, and yellow > 130 HU. Images courtesy of Shane Oberoi and U. Joseph Schoepf, MD. |
At low attenuation levels, the log (representing plaque volume) for each coronary artery and overall were significantly different (p < 0.05) among the three software programs.
Generally, the Vital Images Vitrea software had statistically significant higher log than the other two software programs, TeraRecon's Aquarius and Siemens' Circulation, and Aquarius had statistically significant (p < 0.05) higher volumes than Circulation at each coronary artery as well as overall.
The results in medium attenuation levels were the same as the low levels, except that the volumes for Circulation and Aquarius were not significantly different (p > 0.05) in the LAD and LCX coronary arteries, as shown in the table below.
Results: Automated volumetric data for each software program
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| LAD = left anterior descending artery; RCA = right coronary artery; LCX = left circumflex artery. Data courtesy of Shane Oberoi and U. Joseph Schoepf, MD. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
The automated plaque tools did not always hold the vessel region of interest and diameter constant, meaning that manual adjustments were required on each workstation to ensure that they were consistent.
Measurements of noncalcified coronary artery plaque burden at coronary CTA using automated plaque volumetry do not allow for reproducible quantification across different workstations, Schoepf and colleagues concluded, though repeating the trial showed the results to be reproducible within each analysis platform.
"In itself those tools are reproducible, so you can use these tools to monitor volume changes over time," Schoepf said. "You just need to take care that you use the same tool every single time."
The problem is that people "wander from institution to institution" for their healthcare and, as a result, are treated with many different machines and on different software platforms, Schoepf said.
"What we've seen in calcium scoring is a drive by various industry representatives to come together and develop industry standards to ensure that different workstations really measure the same thing," he said. "So industry can do that, but they may not be aware that different products measure noncalcified plaque very differently."
Considering the importance of noncalcified plaque, that's exactly what industry needs to do, he said.
"We need a similar development in the area of noncalcified plaque," he said.
By Eric Barnes
AuntMinnie.com staff writer
July 20, 2010
Related Reading
Cardiac CAD safely rules out coronary artery disease, June 1, 2010
Symptomatic patients with zero CT calcium scores still have cardiac events, October 2, 2009
CT equivalent to IVUS for culprit plaque detection, December 4, 2008
Coronary artery spasm may trigger acute coronary syndrome, August 15, 2008
MDCT still can't differentiate between noncalcified plaques, January 10, 2006
Copyright © 2010 AuntMinnie.com