Patients undergoing tomotherapy procedures may exhibit signs of post-treatment lung inflammation that differ from those found with more traditional forms of radiation therapy -- a phenomenon that radiologists should be aware of when following up patients, according to South Korean researchers.
Lung inflammation, or radiation pneumonitis, is an early phase of lung injury that occurs three to four months after radiation therapy. Traditionally, the condition appears as ground-glass opacities on CT scans.
But new types of radiation therapy techniques, such as intensity-modulated radiation therapy (IMRT), raise the possibility that radiation pneumonitis could have different manifestations on follow-up CT studies, according to radiologists from St. Mary's Hospital and St. Vincent's Hospital, both hospitals of the Catholic University of Korea in Incheon, South Korea. The researchers warn of this difference in an article published in the September issue of the American Journal of Roentgenology (2009, Vol. 193, pp. W209-W213).
One such IMRT technique is helical tomotherapy, developed to deliver an escalated radiation dose and reduce lung toxicity. It combines the geometry of a diagnostic helical CT scanner with the capability to deliver highly conformal radiation doses distributed in an intensity-modulated fashion.
Because distribution of the radiation dose to the tumor and surrounding lung tissue is more complex and heterogeneous than with conventional radiation therapy, radiologist Dr. Hyun Jin Park and colleagues decided to evaluate the CT findings of radiation pneumonitis that patients developed within three months following tomotherapy treatment.
The authors analyzed CT scans of 77 target lesions in 25 patients who received helical tomotherapy treatment (Hi-Art, TomoTherapy, Madison, WI) for two years starting in January 2005 at St. Mary's Hospital. The patients received the treatment for lung cancer and metastatic carcinomas. The treatment included 50.0 ± 5.99 Gy in three fractions and 40.0 ± 7.03 Gy in 20 fractions. Treatment duration ranged from three to 28 days.
Following treatment, patients were followed with four weekly visits and two additional visits one month apart. Patients had their first follow-up CT scan performed an average of one month following treatment (range, 14 to 90 days) and every two to three months for an additional 11 months. Diagnoses of radiation pneumonitis were made by the consensus of a team of two radiologists and a radiation oncologist.
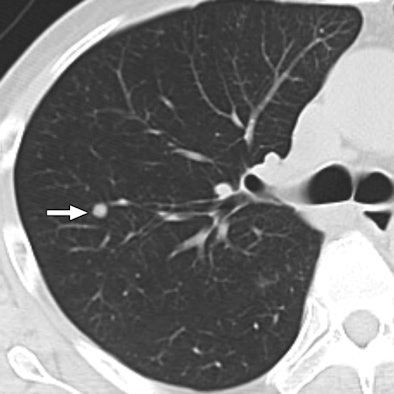 |
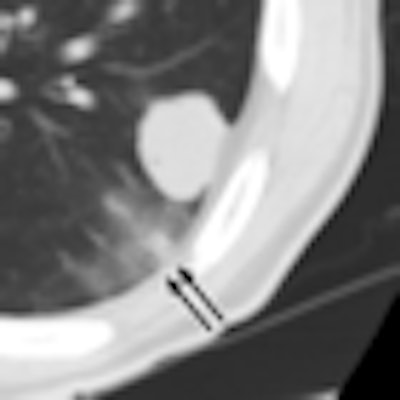
| 47-year-old man with metastatic hepatocellular carcinoma. Above, axial CT scan obtained before tomotherapy shows small well-defined nodule (arrow), target lesion, in right upper lobe. Below, three-month follow-up CT scan reveals focal area of ground-glass attenuation (arrows) around target, representing radiation pneumonitis. All images courtesy of the American College of Radiology. |
 |
Twenty-one of the patients, or 84% of the cohort, had changes in the normal lung around a total of 48 target lesions, or 62.3%. Common findings included irregular shapes and ground-glass attenuation, round shapes, mixed attenuation, and minimal fibrosis.
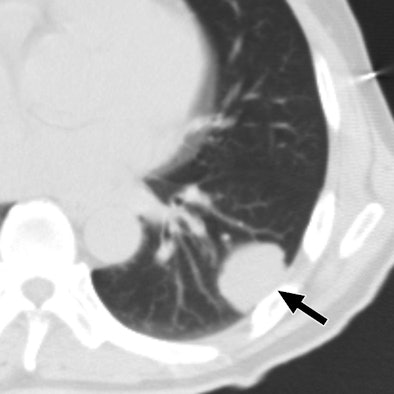 |
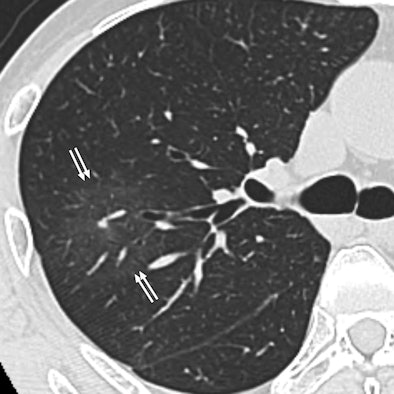
| 60-year-old man with metastatic squamous cell carcinoma from oral cavity. Above, axial CT scan obtained before tomotherapy shows mass (arrow) in left lower lobe, target lesion. Below, one-month follow-up CT scan shows focal ground-glass opacity (arrows) at periphery of target, representing radiation pneumonitis. |
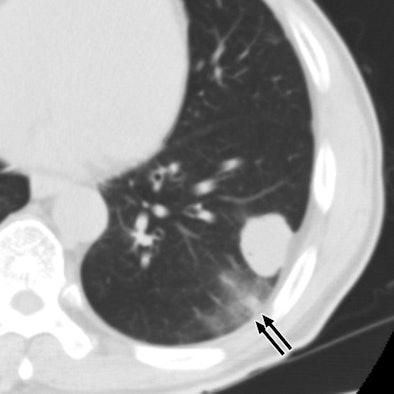 |
The most common CT finding of tomotherapy-induced radiation pneumonitis was a focal area of ground-glass opacities. The radiation pneumonitis also was more prominent in the lower-dose areas than in the higher-dose areas, which the authors believed was a result of increased scatter and leakage and potential double exposure of the periphery of the target area due to respiration.
For the study, two radiologists reviewed the CT exams of patients who developed radiation pneumonitis to determine its density level, if present, and to grade fibrosis as mild to severe. They determined that 65% of the radiation pneumonitis was located on the periphery of the planned target volume, and it was more prominent in lower-dose areas than in higher-dose areas (56%), displaying a pattern that appeared to be off-center relative to the target area.
The authors recommended that future studies include long-term changes shown on CT examinations.
By Cynthia E. Keen
AuntMinnie.com staff writer
August 31, 2009
Copyright © 2009 AuntMinnie.com




















