
"The clinical relevance of small peripheral pulmonary emboli and the need to administer anticoagulants in such cases remain a subject of debate." -- Dr. Martine Rémy-Jardin, Ph.D., et al, Radiology, 2007
Thanks to advanced CT scanners and the watchful eyes of emergency room physicians, the diagnosis of pulmonary embolism (PE) has risen significantly in recent years. Reports of unsuspected PE occurring in as many as 5% of normal patients suggest that doctors are diagnosing cases that would have been missed by ventilation/perfusion (V/Q) scanning or single-slice CT.
Yet despite all the new PE cases doctors are finding, the mortality rate hasn't budged. Researchers from Brown University and Rhode Island Hospital, both in Providence, think they might know why.
At the 2008 RSNA meeting, Jane Suh presented a study she performed with Rhode Island Hospital's radiologist in chief Dr. John Cronan. The study questioned the assumption that all PE are abnormal.
"Current-generation CT scanners allow high spatial and temporal resolution, rapid scanning, and routine visualization of segmental and subsegmental pulmonary emboli," said Suh, who is a medical student at Warren Alpert Medical School of Brown University. "The purpose of our study was to question the theory that all PE are abnormal, and test the hypothesis that small peripheral PE are a function of life."
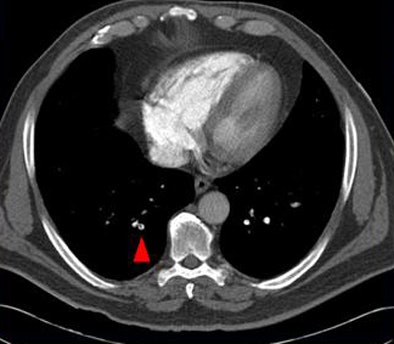 |
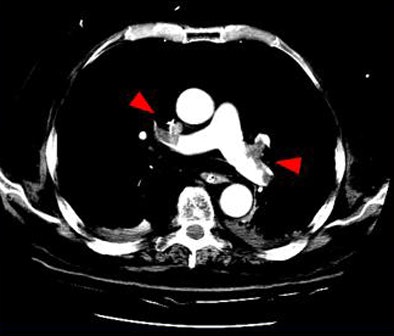
| Above, small peripheral pulmonary emboli are common and are of unknown clinical importance. Image below shows a patient with classic pulmonary embolism, with larger clots involving the central pulmonary vasculature and deep vein thrombosis. All images courtesy of Jane Suh and Dr. John Cronan. |
 |
Part of that normal life involves the constant creation of small blood clots in the peripheral veins that eventually resolve without clinical consequence, she said.
"Cephalic blood flow is received through the veins and forms eddy currents within the valve sinuses," Suh explained. "Small clots can form behind the venous valve cusps, and when you move, for example, from a sitting to a standing position at the end of this session, skeletal muscle contractions cause the veins to wash out and remove these clots."
Finding small clots isn't the problem, but the potential of overdiagnosing and overtreating them is, she said. Current-generation CT scanners allow high spatial and temporal resolution, rapid scanning, and visualization of both segmental and subsegmental pulmonary emboli. A recent study by Ritchie and colleagues found unsuspected PE in 5.7% of inpatients at four- and 16-detector-row CT (Thorax, June 2007, Vol. 62:6, pp. 536-540).
The retrospective study examined the medical records of 1,273 consecutive patients, of whom 101 (7.9%) were diagnosed with pulmonary embolism at CT. The researchers further evaluated 50 patients (24 men, 26 women; ages 21-90 years; mean age, 56.1 years) who also underwent lower-extremity venous ultrasound performed within seven days of the CT.
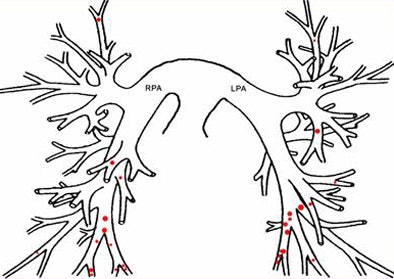
"We reviewed all images and plotted the clots on a diagram of pulmonary vasculature, and also measured the width of the most proximal clot for each patient," Suh explained.
In 32 patients (64%), extensive clotting was noted in the central pulmonary arteries (divisions 1-3), constituting classic PE, she said. In 18 of these cases (56%), deep vein thrombosis (DVT) was also diagnosed with ultrasound.
But in the 18 remaining cases diagnosed with pulmonary emboli, the researchers found only tiny clots in the fourth- through sixth-generation pulmonary arteries ranging in size from 1.5 mm to 4 mm (mean, 2.3 mm). In all, 27.7% of PE cases (28 of 101) at their institution were "dots," with an average width of 2.5 mm, she said.
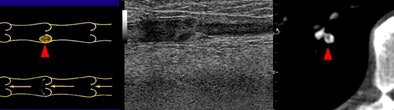 |
| Above, small filling defects, or dots, may represent normal embolic activity originating from the lower-extremity venous valve cusps. Below, location of dots in 27 of 101 patients diagnosed with PE in the study population. |
 |
"Only 11% of these patients [two of 18] had DVT; the majority [15 of 18, 83%] of these patients received anticoagulation treatment just like the patients with classic PE," Suh said.
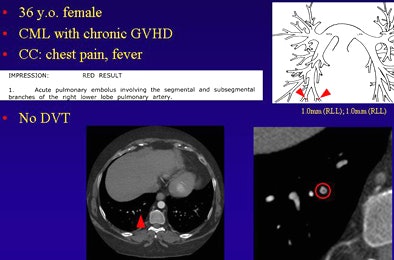 |
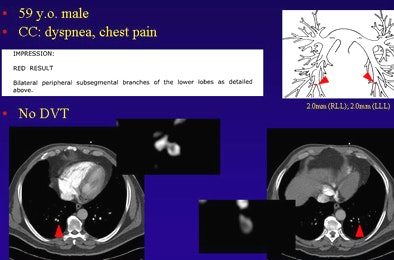
| Dots not clots: Above, thoracic CT angiogram of a 36-year-old woman with chronic myeloid leukemia (CML) and graft-versus-host disease (GVHD) who presented with fever and chest pain. Diagnosed with PE, the report noted 1-mm emboli in the segmental and subsegmental branches of the right lower lobe pulmonary artery. Below, in a 59-year-old man presenting with dyspnea and chest pain, CT angiography detected two 2-mm clots in the peripheral subsegmental branches of the lower lobes. |
 |
"We proposed a theory that dots are small focal and rounded filling defects in the peripheral pulmonary arteries," Suh said. They have a dotlike appearance and are uniformly noted to have blood flowing around them except in the most terminal branches. They are not associated with detectable clot load in lower extremities, she said.
"Dots are not clots in the traditional sense, and we hypothesize that dots represent perhaps normal embolic activity originating from the lower extremity veins."
Healthy people pass these small clots to the lung where they become trapped, Suh said. The lungs have the ability to dissolve small clots by endogenous fibrinolysis, thereby protecting systemic circulation.
"In all, 27.7% of PE cases [28 of 101] were dots," she said. "We learned that dots are far more common today due to advances in CT technology, and we will need further studies to determine their significance."
Pending further study, and considering the risk of bleeding associated with thrombolysis, the results suggest that focal "dotlike" filling defects in the peripheral pulmonary artery in the absence of detectable clots in the lower extremities should not trigger a therapeutic regimen for PE, she said.
By Eric Barnes
AuntMinnie.com staff writer
February 4, 2009
Related Reading
Dual-energy CT helps distinguish PE from other perfusion defects, December 2, 2008
Multislice CT plus D-dimer testing sufficient for excluding pulmonary embolism, April 21, 2008
Study reinforces V/Q, PIOPED II guidelines for PE during pregnancy, February 15, 2008
Multicenter trial supports CTPA versus V/Q for PE, December 18, 2007
Low-dose CT yields equivalent value for PE in pregnancy, November 27, 2007
Copyright © 2009 AuntMinnie.com




















