
A computer-aided matching program can yield a high rate for matching metastatic pulmonary nodules on clinical series CT scans, provided that lung findings and lung expansion between the serial scans are relatively unchanged, according to an article in the November issue of the American Journal of Roentgenology. Matching rates decreased significantly with substantial interval changes in the lung and a larger number of nodules.
"Thus, in the current implementation, application of the automatic matching algorithm seems most appropriate for follow-up images obtained in cases with similar conditions of surrounding lung disease and similar inspiratory states," wrote a research team led by Dr. Kyung Won Lee from the Mallinckrodt Institute of Radiology in St. Louis.
The researchers sought to evaluate the performance of a computer-aided program that provides automated matching of metastatic pulmonary nodules imaged with two serial clinical chest CT studies. Cases from 30 patients with metastatic pulmonary nodules depicted on two serial clinical multidetector-row (MDCT) scans (16- or 64-slice MDCT, 5-mm section thickness) were included in the study (AJR, November 2007, Vol. 189:5, pp. 1077-1081).
The researchers then selected a maximum of 10 well-defined nodules per patient from each baseline CT scan for a total of 210 nodules, which were then evaluated for matching detection in follow-up CT using LungCare VB20 software (Siemens Medical Solutions, Malvern, PA). The study team also visually assessed substantial changes in lung findings and lung volumes between serial scans, as well as analyzed the effects of interval lung changes and location, size, and total number of lung nodules on the matching rate.
The software turned in a median nodule matching rate of 87.5% (range: 0 to 100%) and an overall matching rate by nodule of 66.7% (140 of 210). In the 23 patients with relatively unchanged lung findings, the software matched 122 of 148 (82.4%) nodules. In contrast, the software only matched 18 of 62 nodules (29%) in seven patients with substantial interval changes (p < 0.001).
The researchers also found a decreased matching rate with an increased total number of nodules per lung. Matching was successful for 31 of 36 nodules in cases with 10 or fewer nodules per lung, 60 of 73 nodules for 11-50 nodules per lung, 33 of 47 nodules for 51-100 nodules per lung, and 16 of 64 nodules for more than 100 nodules per lung (p < 0.001). The authors did not find a significantly different matching rate by location or nodule size.
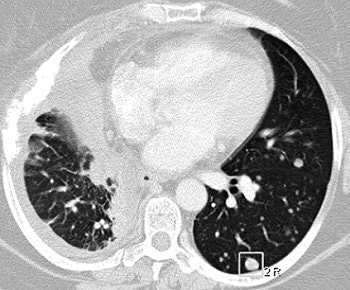 |
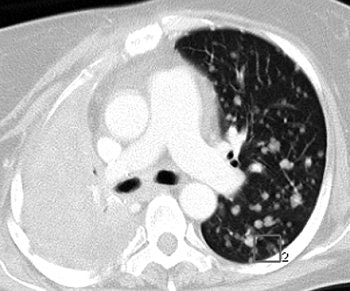
| A 47-year-old woman with numerous metastatic nodules from small cell lung cancer in right lung and unmatched nodule in superior segment of left lower lobe. Above, transverse CT image shows baseline findings. Below, transverse reformatted CT image shows follow-up findings. Overall matching rate was 0 (0/10). Infiltration of lung cancer was markedly increased, with complete collapse of upper lobe of right lung during interval. |
 |
| Lee KW, Kim M, Gierada DS, and Bael KT, "Performance of a Computer-Aided Program for Automated Matching of Metastatic Pulmonary Nodules Detected on Follow-Up Chest CT" (AJR 2007; 189:1077-1081). |
It appears the current automated matching program would allow faster assessment of whether metastatic disease has changed than an approach relying on manual matching of nodules, according to the researchers.
"Although the matching rates are reduced in some circumstances, the program seems to match enough nodules to be of benefit in the sense that it can reduce the radiologist's time spent determining whether change has occurred," the authors wrote. "Most of the unmatched nodules were found within three sections of the nodule to be compared, potentially reducing the search time even for cases in which a nodule selected for follow-up comparison is not perfectly matched."
The authors stated that further study is required for assessing the clinical benefits of automated nodule matching.
"The radiologist's attention to the accuracy of the matching result for each nodule is still recommended in the clinical setting," the authors concluded. "The importance of automated nodule matching to clinical care and workflow remains to be determined."
By Erik L. Ridley
AuntMinnie.com staff writer
November 16, 2007
Related Reading
Measuring lung nodule growth beyond variability, November 5, 2007
Radiologists no match for nodule measurement software, August 31, 2007
Part I: Automated CT lung nodule assessment advances, April 17, 2006
Copyright © 2007 AuntMinnie.com





















