Ground-glass opacities (GGOs) are different from solid nodules found at thoracic CT, and they need more frequent follow-up.
In a talk at the 2007 International Symposium on Multidetector-Row CT in San Francisco, Dr. Ella Kazerooni, professor and director of cardiothoracic radiology at the University of Michigan in Ann Arbor, reviewed the why and how of GGOs, a troublesome result of CT screening that radiologists are encountering more frequently as more smokers and former smokers are screened.
At CT, ground-glass opacities can be diffuse (a common finding in interstitial lung disease), multifocal, or focal, and they can represent a wide range of etiologies, Kazerooni said. Focal GGOs -- those with a ground glass or nonsolid component -- have a far greater malignancy rate than solid nodules, according to a number of studies.
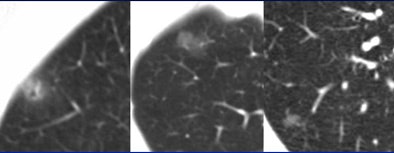 |
| Three focal ground-glass opacities (GGO) show the variety of presentations at MDCT. The lesion at left has a hazy appearance, with uniform surface lucency. The nodule in the center image is more subtle; no architectural distortion can be seen in the surrounding parenchyma. The GGO at right is rounder and smaller. All images courtesy of Dr. Ella Kazerooni. |
In the first ELCAP lung cancer screening trial, Henschke et al "found 233 cancers in the first 1,000 patients," Kazerooni said. "Only 8.4% of the solid nodules proved to be cancer, 18% of the completely (nonsolid) GGO lesions were cancer, and 63% of the mixed (part-solid) nodules proved to be cancers -- these are the most concerning."
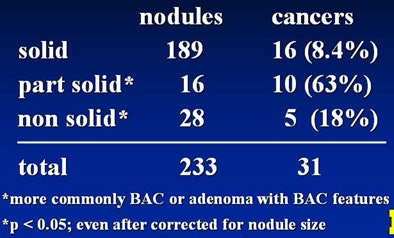 |
| Among 233 cancers detected in the first 1,000 patients of the ELCAP study, Henschke et al found markedly higher rates of malignancy in mixed-composition part-solid nodules. AJR, May 2002, Vol. 178:5, pp. 1053-1057. |
When malignant, GGOs are either bronchoalveolar cell (BAC) carcinomas, adenomas, adenomas with BAC features, or occasionally a lymphoma, Kazerooni said. "But there are other things they can be, including atypical adenomatous hyperplasia (AAH), infection, inflammation or postinflammatory fibrosis, or hemorrhage," she added.
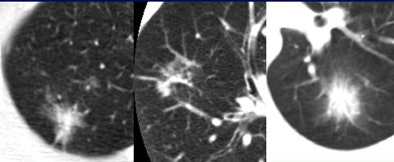 |
| Part-solid nodules with a ground-glass component have the highest rate of malignancy, according to several studies. |
In a 1990 paper, Weng et al described atypical adenomatous hyperplasia as "peripheral focal proliferation of atypical cuboidal and columnar epithelial cells replacing pre-existing alveolar or bronchoalveolar epithelium, giving rise to a gland-like appearance" (Histopathology, January 1990, Vol. 16:1, pp. 101-103).
Researchers from Shinshu University School of Medicine in Matsumoto, Japan, took another look at AAH in a large CT screening study, describing it as "atypical epithelial cell proliferation along slightly thickened alveolar septa." Among 17,919 CT lung cancer screening subjects, the researchers found 10 AAH lesions. The lesions ranged in size from 6 x 6 mm to 15 x 17 mm. All were round with smooth borders and all demonstrated a ground-glass CT attenuation between -500 and -760 HU at MDCT.
"Whereas it is often easy to differentiate these nodules from inflammatory and benign lung lesions, histopathological examination remains at present the only method to differentiate AAH from lung cancers," Kawakami and colleagues wrote (European Radiology, April 2001, Vol. 11:5, pp. 811-814).
Kodama et al examined 19 patients with GGOs that persisted for more than two years, including 11 screened subjects, seven followed up after cancer resection, and one patient with a GGO detected incidentally (Annals of Thoracic Surgery, February 2002, Vol. 73:2, pp. 386-392).
The lesions ranged in size from 4-18 mm at detection (mean 8.6 mm). At follow-up, eight patients showed no change, while GGOs grew in 11 (n = 6, < 5mm; n = 5, > 5mm). Resection in 10 patients yielded five adenomas, three with lymphoproliferative disorders, one AAH, and one focal fibrosis. Benign AAH was proved in an additional nine patients, Kazerooni said.
Correlation of AAH with histology shows the characteristic "gland-like epithelium and air-filled spaces" of AAH, which accounts for why it's not very subtle on CT images.... And you can't tell it from BAC," Kazerooni said.
Writing in Chest, Nakata et al examined 43 patients who underwent thoracoscopic biopsy of persistent focal GGO 2 cm or smaller after a mean 3.7 months observation. They found malignancies in 34 of 43 patients, including 23 BACs, 11 adenocarcinomas, mixed subtypes, and all patients were lymph-node negative (Chest, May 2002, Vol. 121:5, pp. 1464-1467).
Importantly, all GGOs 1 cm or larger were malignant, and 93.3% of GGOs with a solid component were malignant.
"One thing we tend to do with patients with ground-glass nodules is to follow them, which is different from patients with purely solid nodules," Kazerooni said. Another difference: ground-glass nodules that aren't cancer could have inflammatory or infectious origins.
"One way to clear it up for the patients and the referring physician very quickly is to suggest a course of antibiotics, with a repeat CT at a short interval -- as short as four to eight weeks," she said. "If the nodule goes away completely, the physician and the patient can be assured that the nodule is not malignant."
Given GGOs overall higher rate of malignancy, Kazerooni recommended follow-up CT at three months, or a course of antibiotics with follow-up CT at four to eight weeks.
By Eric Barnes
AuntMinnie.com staff writer
August 22, 2007
Related Reading
Divergent research on CT lung screening sparks more debate, fewer answers, April 19, 2007
CT screening may not improve lung cancer survival, March 7, 2007
CT lung cancer screening reduces mortality, October 26, 2006
Ultralow-dose lung MDCT may still find ground-glass lesions, November 30, 2005
Emphysema alters CT appearance of benign nodules, May 4, 2005
Copyright © 2007 AuntMinnie.com




















