If physicians were compelled to face all the factors that influence their workload, they might be tempted to head home and go back to bed.
The typical to-do list would include:
- Scheduling
- Registration
- Front and back office flow
- Documents
- Information systems
- People
- Travel
- Preferences
- Style
- Rules and regulations (HIPAA, Medicare)
- Locations
- Supply and demand
- Reimbursement
Fortunately, most doctors don't have to keep an eagle eye on these workload issues because that's what practice managers do. And one way managers can keep track of productivity is by implementing a physician workload management system.
This can be done in a number of ways, according to healthcare consultant Melissa Dill. The key is to apply a consistent methodology, and make sure it is accepted by all involved parties.
Dill, who is with Health Evolutions of Indianapolis, presented her ideas for managing physician workload in a poster at the 2004 Medical Group Management Association (MGMA) meeting in San Francisco.
Before any system can be set up, "you certainly have to have the physician buy-in. There has to be consensus that they want to implement some way to measure their productivity," Dill said in a telephone interview with AuntMinnie.com. "Involving the physicians in the development of the system is another way to enhance your ability to succeed with implementation. Finally, make sure that they understand the system."
There are three options for measuring productivity, according to Dill. One is relative value units (RVUs), which are based on the resources used for furnishing physician services. Fifty-five percent of RVU is allotted to workload, 42% to practice experience, and 3% to liability insurance.
The second option is an internal comparative approach that "compares individual physician productivity within a given practice group/area to one another." Productivity expectations are also based on historical data.
The third is an external comparative approach in which individual MDs are compared to external benchmarks. This last option uses a compensation-to-production/collections ratio, which compares compensation dollars to production/collection dollars. This final method does require a well-honed collection effort on the part of the practice or department, Dill said.
In her presentation, Dill focused on RVUs, which were first introduced into the practice management lexicon in 1992, and adopted by the U.S. Centers for Medicare and Medicaid Services (CMS) two years later. The RVU model calculates payments by multiplying the combined costs of a service by a conversion factor (a dollar amount determined by CMS). Payments are also adjusted for geographic differences in resource costs.
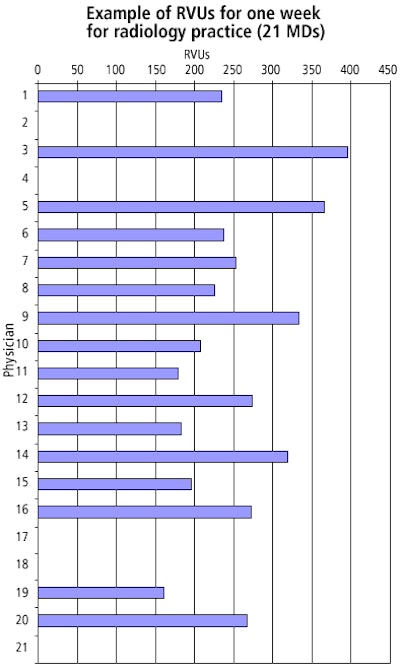
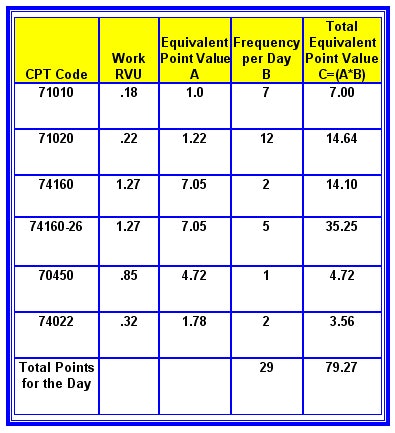
Dill emphasized the importance of everyone in the practice understanding the mechanics of RVUs. In her MGMA presentation, she offered examples of how to set up an RVU-based performance system from a project with a 21-person radiology facility. Dill said she found a considerable amount of confusion about RVUs before the process even began.
"We did provide quite a bit of education on what an RVU meant, and how it was developed," she said. "There was a lot of misinformation about RVUs. People were talking back and forth, and suddenly one person's misunderstanding of RVUs became a group's misunderstanding of it."
Once everyone is on board with the basics, RVU reporting becomes a component of a workload allocation system. Dill laid out the steps for this system, with each of the following segments assigned to a particular person in the practice and a target date of completion:
- Gain consensus in facility to create allocation system.
- Present system to physicians.
- Gain consensus regarding daily point targets.
- Determine software capabilities for reporting RVUs.
- Develop reporting mechanism.
- Review process.
- Set implementation date.
- Implement workload allocation system.
A radiology practice that she consulted with chose to use a daily point targets system. Rather than forcing the physicians to remember the actual RVUs, the group opted for a more accessible method.
"They said, 'A physician is not going to remember that a CPT code for x-ray (has) a work RVU of 0.18.' But they would remember that a chest x-ray is equal to one point," Dill explained. "They felt that the chest x-ray was the basic procedure that they all do so the chest x-ray equaled one point, and then everything else was relative to the chest x-ray."
The chart below illustrates a typical day in the life of a radiologist based on the RVU productivity system:
 |
The simplified point system is optional, Dill said, but for this particular group, it was a necessary aid for tracking workload assessment. For example, an HCPC 71010 (chest x-ray) would be equal to an RVU of 0.18, or one point in the practice's internal system. In comparison, an HCPC 74160 (abdominal CT with contrast) would be equal to 1.27 points.
"The purpose ... was to show that certain procedures take more resources, or, in effect, are harder to do," she said.
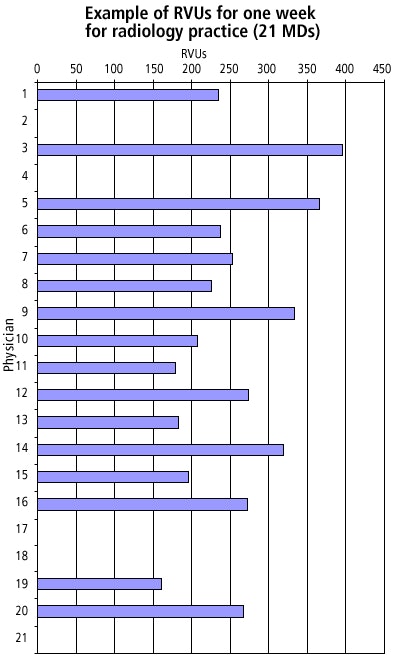 |
Dill cautioned that incorporating a workload assessment system won't happen overnight. At the radiology practice she referred to, it has taken several months to fine-tune the system and begin the process, she said.
However, once in place, the system may have the added benefit of moderating any workload-related friction or animosity. Such was the case at the radiology group, Dill said.
"There was an impression that certain physicians weren't pulling their weight, and that there were others who were doing more than their share. When we actually came up with a concrete (productivity) system to look at, some of (those impressions) were validated and some were not. There were some surprises in there," she said.
While some practices may consider it taboo to publicly address workload issues, in the long-term it can only improve their output. "When you are not talking openly about (workload) information, a group runs the risk of there being a lot of misconceptions about who is busy and who is not," Dill said. "Then it needs to be addressed, and (workload assessment) is one way that we did it."
By Shalmali Pal
AuntMinnie.com staff writer
October 29, 2004
Charts courtesy of Melissa Dill.
Related Reading
Medicare database shows cardiologists driving up imaging costs, January 9, 2004
Hospital-physician collaboration can alleviate radiologist shortage, March 26, 2003
Copyright © 2004 AuntMinnie.com