The basic concept of a breast tissue marker is simple and not terribly new. After all, metallic markers have been used for more than three decades to flag gynecologic and brain tumors for radiation treatment.
Yet just a few years ago, there were no markers designed specifically for use in breast tissue. Now there are several on the market, thanks to the revolution in cancer detection and breast-conserving treatments.
Trends in the diagnosis and treatment of breast disease have spawned demand for markers that are easily deployed, visible on sonography and mammography without causing significant artifacts on MRI, and resistant to dislocation. However, the technology is straightforward enough that commercial systems face serious competition from inexpensive, do-it-yourself solutions.
Clinical applications
The late development of breast tissue markers parallels the relatively recent changes in breast biopsy practices, according to observers.
"The need (for specialty breast tissue markers) was always there at some level," said Dr. Eric Rosen, an assistant professor of radiology at the Duke University Medical Center in Durham, NC. "But with the use of larger-gauge biopsy needles and vacuum assistance, it’s more frequent that we’re removing the visible portion of a mammographically detected, nonpalpable lesion with our percutaneous biopsy."
"The area of tissue removed is a 10 to 12 mm sphere, and that is a significant enough volume that even if the entire lesion is not completely removed, knowing where that sphere was taken from can be important," said Dr. Ralph Smathers, founder of the Mammography Specialists Medical Group in Los Gatos, CA.
Surgeons can get cranky when asked to follow up on a cancerous lesion that is no longer visible, Smathers said, while a metallic marker gives them something to latch onto -- sometimes literally.
Rosen estimates that nearly 500,000 vacuum-assisted biopsies are performed each year. Procedure volume has increased enormously since 1996, when the 14-gauge Mammotome biopsy system was introduced.
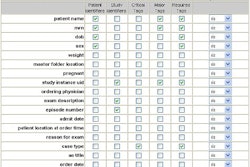
Dr. Frederick Margolin, director of the Breast Health Center in San Francisco, contends that the vast majority of stereotactically guided breast biopsies in the U.S. are now performed with an 11-gauge Mammotome device and denoted with a MicroMark breast tissue clip, both marketed by Ethicon Endo-Surgery, the Cincinnati-based subsidiary of health products giant Johnson & Johnson of New Brunswick, NJ.
There are ways to identify a biopsy site without a marker, like using ultrasound to spot a lingering hematoma. "But the simplest and most straightforward way is to leave a mark," Margolin said. "So we do that whenever we’ve removed all of the calcifications."
"I think we now use a marker in the vast majority of cases, probably 90%," echoed Smathers. "The only time I would not leave a marker is if I had a very large lesion where I was just taking a sample from the edge."
Another trend spurring the need for markers is the increasing use of neoadjuvant chemotherapy to shrink breast tumors prior to surgery. Because chemotherapy can reduce tumors to near invisibility, many facilities now implant tissue markers at the tumor site prior to treatment, knowing that the marker will still highlight the cancerous region at subsequent surgery.
Many radiologists are also deploying markers during ultrasound-guided biopsies. "It’s quite frequent that you’re biopsying something under ultrasound, which you believe correlates with the finding on the mammogram," Margolin explained. "It’s very, very helpful to prove that by leaving a mark at the site of the ultrasound-guided biopsy and then doing a mammogram."
Rosen opts against using markers with ultrasound biopsies, since those procedures generally don't excise lesions and he is concerned about overuse of metallic markers.
"We know from experience with retained needle wires from needle localization that sometimes these wire fragments, when left in the breast, can migrate, even out of the breast," he said. While there is no comparable long-term data on metallic clips, "one would not want to put a piece of metal in the breast -- that could potentially migrate out of the breast -- when it wasn’t really necessary."
That concern sounds unwarranted to Dr. Richard Chesbrough, a radiologist with the Henry Ford Health System in Detroit and inventor of the UltraClip breast-marking device.
The localization cases were rare, he says, and "a straight piece of wire doesn’t have any impediment to working its way through the tissue." In contrast, the metallic shapes used in breast markers will fibrose in place and are unlikely to move much, Chesbrough maintained.
Technology issues
A few case reports of severe dislocation have been published, but the medical literature on markers is mostly about migration measured in millimeters -- movement that can be major when one is trying to address a small cancerous area with breast-conserving therapy.
In a retrospective analysis of 111 biopsies and clip deployments at Duke, Rosen and co-author Thuy Vo found that 31 clips (28%) were more than a centimeter from the target on at least one post-biopsy image. Eighteen of these mismarked biopsies involved lesions that were malignant or atypical and required excision.
Much of this commonplace migration is apparently due to the "accordion effect" -- the magnification of discrepancies between the marker and biopsy site as compression is released. Several studies have found that clip migration most often occurred in the z-axis, the plane perpendicular to that used for compression during biopsy, according to Rosen and Vo.
The Duke researchers recommend routine orthogonal-view film-screen mammograms after biopsy to document any error in clip placement.
"This documentation is particularly important if needle localization is performed at another institution or by another radiologist who is not familiar with the case," the authors wrote. "It is also important in cases in which the lesion is excised at stereotactic biopsy and residual hematoma and/or air is no longer identifiable at the time of needle localization" (Radiology, February 2001, Vol. 218:2, pp. 510-516).
Rosen and Vo also suggest that optimizing the quality of stereotactic imaging could reduce unnecessary marker deployments.
"The stereotactic images obtained after biopsy...were often limited due to their small field of view, poor compression, overlapping shadow of the biopsy probe, and obscuring hematoma," they wrote. "Because the decision whether to deploy a clip was based on the assessment of stereotactic images, we found that many clips were placed when the lesions were not visibly excised."
Vendor systems
Concern about marker migration has also spurred innovation in marker technology, as some observers believe the accordion effect is exacerbated by metallic clips that attach themselves to tissue at the border of a biopsy cavity.
Smathers served as a consultant on and tester of one alternative, the Vivant Medical Biopsy Marker System (Vivant Medical, Mountain View, CA). The Vivant marker is a titanium ring surrounded by a bioabsorbable collagen cylinder, which Smathers reviewed in a short article this year in the American Journal of Roentgenology (February 2003, Vol. 180:2, pp. 355-356).
"Portions of the collagen cylinder on both sides of the marker expand to absorb fluid and stabilize the marker within the cavity," he wrote. "This feature tends to place the metallic marker centrally in the biopsy cavity and to make the marker resistant to migration."
However, since the Vivant system isn’t being marketed as yet, Smathers is using MammoMark (Artemis Medical, Hayward, CA), a very similar system. Rosen is another MammoMark fan.
"The thing I like about their clip is that instead of attaching to the side wall of the biopsy cavity, the collagen plug goes into the cavity and expands from the blood and fills. It reduces the initial accordion effect," Rosen said. "Also, there’s a potential hemostatic benefit from the collagen because it induces blood clotting."
Rosen also appreciates that the metallic portion that remains from the MammoMark is titanium, which produces very little artifact on MRI. All of the current marker systems leave some sort of radiopaque metal for long-term mammographic visibility.
Smathers said that while he hasn’t heard of a case where a marker rendered an MR exam worthless, the issue of artifact will become more important with higher-field imaging. In the short term he is more concerned about a marker site that requires another biopsy, as the tiny metallic markers can get into the notch of a biopsy needle and jam it.
Stainless-steel markers are deployed in the systems offered by SenoRx of Aliso Viejo, CA, which also markets the SenoCor 360 core-needle biopsy device, as well as biopsy and localization wire guides.
The company currently offers three biopsy site-marking systems: Gel Mark, Gel Mark Ultra, and Gel Mark UltraCor. All three use plunger-driven disposable applicators to inject the biopsy site with fewer than a dozen sonographically visible gelatin pellets, one embedded with a stainless-steel marker that will resorb within six weeks.
Smathers noted that the Gel Mark systems are appreciated for the superior sonographic visibility provided by the multiple pellets. "On the other hand, I’ve heard some criticism about those little marks going back down the needle track because they’re so small." he said.
SenoRx advertises that its Gel Mark systems are compatible with the Mammotome biopsy system. As noted previously, the makers of the Mammotome also offer their own Mammotome-compatible system, MicroMark II.
Then there is UltraClip, which is designed primarily for placement of clips after ultrasound-guided core biopsies. It is distributed by InRad of Kentwood, MI, which also markets a variety of localization wires, core biopsy needles, aspiration needles, and other devices.
Chesbrough said he came up with the UltraClip concept in 1999 as his use of ultrasound-guided biopsy increased. Rather than being deployed through the inner lumen of a mammotomy needle, the UltraClip marker is pre-loaded in a stiff 17-gauge needle that follows the track made by the biopsy needle.
"One reason people used the larger (mammotomy) needles was they needed to leave a clip behind, or they felt they did," Chesbrough said. His invention allows radiologists to deploy a clip in five seconds, he said, while using a biopsy method that is quicker, less expensive, and less invasive.
UltraClip is currently a 3-mm steel tissue marker, although a newer version of the marker due out by RSNA will be made from titanium and coated with a material that enhances its echogenicity.
Margolin said he’s been using UltraClip "quite successfully." His summary: "It’s quick and easy; you take your biopsy needle out and put this one in."
Click here for a list of clip marker vendors.
Off-label bargains
But Margolin pointed out that the downside of these commercial clip offerings is price. Prices go from $75 and below per unit for MammoMark. That’s why he’s often deploying his own metallic markers, at a cost of around $4 each.
His approach involves taking a U-shaped clip used by surgeons to ligate very small vessels and crimping it into a marker that fits inside the bevel of an 18-gauge spinal needle when the center stylet is removed. When the stylet is reinserted into the needle, the marker is deployed. Margolin pre-crimps his markers, and then sends them to central supply at the California Pacific Medical Center in San Francisco to be sterilized and packaged in pairs for use in future biopsies.
Margolin said he was inspired by an RSNA presentation made years ago by a Montreal group, but the Canadians apparently never published anything on their efforts. Margolin and his colleagues at San Francisco’s Breast Health Center recently described their technique and experience in The Breast Journal (May 2003, Vol. 9:3, pp. 226-230).
"We’ve actually used this in about 25 ultrasound-guided biopsies and about 100 stereotactic biopsies," Margolin said. His group has also written a paper for an upcoming issue of AJR comparing their do-it-yourself approach with the MicroMark device, finding that the accuracy of positioning and stability over time were equivalent for the two markers.
Meanwhile, a group from the M.D. Anderson Cancer Center in Houston has also described deployment of their own blunt metallic markers under ultrasound guidance to localize breast tumors before beginning preoperative chemotherapy. The markers were fashioned by cutting 5-mm segments from a 23-cm stainless-steel 18-gauge wire. The group found no documented migration of the markers after deployment (Radiology December 1999, Vol. 213:3, pp. 895-900).
M.D. Anderson is now a big consumer of UltraClips, according to Chesbrough, who doesn't have a problem with "homemade" solutions. "We did that before we had the UltraClip," he said, often using embolization coils that weren't that cheap.
Another factor to consider, said Chesbrough: "If it takes you a few minutes crimping the wire, what’s your time worth?"
Rosen sees no need to create off-label replacements for clips he regards as "not very expensive" at $75 each. But Smathers shares Margolin’s cost concerns -- perhaps reflecting a split based on practice type and/or West Coast location.
"We would like to use the top-quality commercial markers, but there is tremendous pressure to do things cheaper," Smathers said. "Price is a definite issue these days with the reimbursement."
"Some of the insurers actually have paid so little that they have not covered our cost for the needle and marker combined, which is really an outrageous state of affairs," he stated. "These kinds of biopsies are huge improvements for patients and they have saved many healthcare dollars, because every time you do a large-core vacuum-assisted biopsy, you’re saving an entire surgery."
Reimbursement
Margolin is happy to forgo his own clips, "when I want to do the quickest and easiest thing first -- situations where I’m pretty comfortable that the cost will be covered by insurance."
While many biopsy patients would be too young to be covered by Medicare, the U.S. Centers for Medicare and Medicaid Services issued a new code (CPT 19295) in 2001 covering the placement of localization clips.
But whatever the reimbursement, it is clear that markers have become critical in the diagnosis and treatment of breast cancer. "They fill a very important niche," Rosen said.
Margolin concurred. "It’s pretty much standard of care, now that these things are available."
By Tracie L. ThompsonAuntMinnie.com contributing writer
August 26, 2003
Related Reading
US-guided biopsy marker takes clear aim at breast lesions, May 5, 2003
U.K. researchers explore reasons for biopsy clip movement, March 8, 2003
New adjunctive breast techniques improve positive biopsy rates, February 25, 2003
Post-biopsy gel marker stays put on mammographic follow-up, December 5, 2002
Breast biopsy technology evolves at a rapid pace, May 16, 2002
Copyright © 2003 AuntMinnie.com