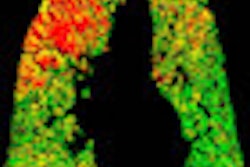
A study published online September 3 in the New England Journal of Medicine found that pulmonary artery enlargement as seen on CT scans is closely correlated with the development of exacerbated chronic obstructive pulmonary disease (COPD) symptoms, providing a potentially strong predictor of symptom onset.
Researchers from the University of Alabama at Birmingham and other institutions found that a pulmonary artery (PA) diameter measurement larger than the aorta (A) diameter at CT, or PA:A > 1, was associated with severe exacerbations of COPD, both at presentation and in terms of future risk of severe symptoms.
"We found that a PA:A ratio of more than 1 at baseline was associated with future exacerbations of COPD, particularly those requiring hospitalization," wrote Dr. J. Michael Wells and colleagues. "The metric is particularly valuable given that the measurement of this ratio requires minimal training and, when measured at the pulmonary artery bifurcation, appears to be reproducible" (NEJM, September 3, 2012).
Increases in dyspnea, cough, or sputum production requiring changes in management qualified as COPD exacerbations in the study. These exacerbations are often triggered by new strains of bacteria, viral infections, or exposure to pollution, the authors wrote. COPD patients often experience increased respiratory symptoms due to subclinical or overt cardiovascular events as well.
Better tools are needed to predict exacerbations, they wrote, particularly in cases requiring hospitalization. The study aimed to explore the association between pulmonary artery enlargement and exacerbations in 3,464 smokers and former smokers with COPD. Wells and colleagues examined the association between PA:A > 1 and a history of hospitalization for COPD exacerbation, going on to examine the utility of this association.
The researchers found a significant association between PA:A > 1 and a history of COPD exacerbations at the time of enrollment in the trial, with an odds ratio of 4.78 (p < 0.001). In addition, a PA:A ratio > 1 was associated with an increase in future exacerbations in both the study cohort (odds ratio, 3.44) and another cohort used for external validation (odds ratio, 2.80).
Pulmonary artery enlargement detected by CT was strongly associated with severe exacerbations of COPD, Wells and colleagues wrote of the results. Many patients presenting with symptoms consistent with severe COPD exacerbations have poor clinical outcomes, and CT is useful in identifying this population at risk, according to the authors.
"Though congestive heart failure, sleep apnea, and thromboembolic disease were not independently associated with exacerbations, the value of the PA:A ratio may be due in part to its capacity to identify patients who have pulmonary vascular disease as a result of these disorders and who are at particular risk for cardiovascular triggers of exacerbation," they wrote. Elevated PA:A may also help identify patients with underlying emphysema.
Several causes or a combination of causes such as resting hypertension, undiagnosed cardiovascular disease, or local disease may be responsible for the PA enlargement at CT, they wrote. Future studies could be designed to test a variety of anti-inflammatory agents for their ability to calm symptoms in patients prone to COPD exacerbations.
The use of a size ratio with the aorta rather than pulmonary artery size alone renders the test amenable to different patient sizes, they added, and the test is simple enough to perform with routine CT images obtained without contrast or the use of special software.