Peripherally inserted central catheters have been a fast-growing part of medicine for more than a decade now, with hospital radiologists playing a critical role in confirming the placement of these devices. Yet despite years of experience, a globally standardized approach to imaging of PICC placements remains elusive.
One indisputable aspect of PICC placements, however, is their medical importance. Given the usefulness of vascular access for the central delivery of medications, blood products, and fluids, researchers continue to explore ways to minimize complications and optimize placement of these so-called "long lines."
After a patient with a peripherally inserted central catheter (PICC) nearly died on his way to the x-ray department, Children's Hospital in Cincinnati began performing all PICC insertions with fluoroscopy. Many facilities serving adult patients have also moved to fluoroscopic confirmation, according to Dr. John Racadio, the hospital's interventional radiology chief.
Based on the patient information posted on various hospital Web sites, however, the post-insertion chest x-ray remains a viable option at many facilities. (The use of ultrasound to guide the catheter insertion is also a hot topic in the medical literature and on Web sites that offer training for nurses specializing in PICC placement.)
In particular, neonatal specialists outside the U.S. are still seeking to improve x-ray confirmation of PICC placements in the littlest patients. A recent study in New Zealand found the use of contrast at radiography improved the likelihood of visualizing the catheter tip in neonates.
Another study in the same journal argued that PACS could obviate the need for contrast or repeated films, as soft-copy reporting of radiographs "significantly improves the accuracy in determining neonatal long-line position and tip," according to the authors (Archives of Disease in Childhood, Fetal Neonatal Ed, January 2004, Vol. 89:1, pp. F41-F45).
"This may have implications for the provision of CR/PACS access on the neonatal unit," the group concluded, as "[a]ccess is of particular importance out of normal working hours and when immediate radiological review may not be possible."
Fluoroscopy is often not viewed as an option.
"The reason is simply practicality," observed Dr. Jane Harding, a professor of neonatology at the University of Auckland in New Zealand. "(Fluoroscopy) would entail moving the babies to a suitable facility, and most babies who need long lines are too ill to move."
"I know of no neonatal unit anywhere that uses fluoroscopy for placement of percutaneous long lines in neonates," she added.
But as always in medicine, practices differ by location.
Children's Hospital in Cincinnati already performs many neonate PICC placements in its interventional suites, according to interventional chief Racadio. Within the next year or two, Children's will also install a c-arm fluoro machine in a dedicated procedure room located in the neonatal intensive care unit.
 |
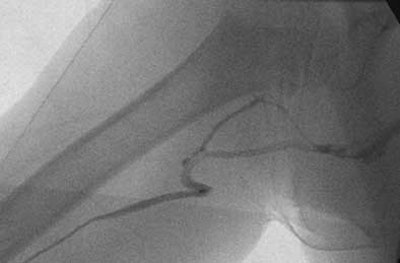
| Fluoroscopic spot image from a PICC placement at Children's Hospital in Cincinnati involving a child who has undergone prior PICC placements. After gaining ultrasound-guided access to the right basilic vein, the catheter would only thread to the upper arm, at which point it would buckle. Contrast injection revealed venous tortuosity. All images courtesy of Dr. John Racadio. |
Clearly, part of what drives the availability of fluoroscopy-guided PICCs is the willingness of interventionalists to support such services. Racadio's interest includes ongoing research to check his beliefs regarding fluoroscopy versus radiographs.
Bedside PICC placements can be slowed by major misfires, with catheters threading up a jugular vein or across to the other brachial arteries rather than going down to the superior vena cava. But a more vexing issue may be getting the catheter tip into optimal position.
"More and more, the articles that are coming out are showing that the tip location is very important, and really to aim for that lower third of the superior vena cava is optimal if you want to have the safest PICC and the best chance for not having complications," said Racadio.
"In order to get that precise position -- if you’re repositioning the catheter blindly on the (hospital) floor, just kind of relying on chest x-ray interpretation -- sometimes these PICCs could go on forever," Racadio said.
 |
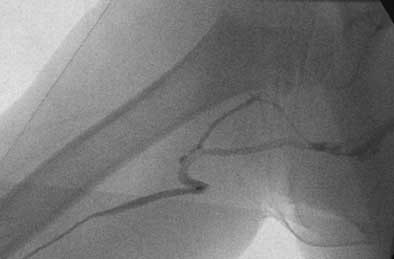
| Dr. John Racadio placed a 0.014-inch hydrophilic guidewire through the catheter and maneuvered through the tortuosity into the superior vena cava, as shown in the final placement image here. "You can imagine how this PICC placement would have been impossible if the attempt were at the bedside without fluoro assistance," noted Racadio. |
In the sentinel mid-1990s incident at Children's, a child whose catheter was placed too deep in his right atrium went into arrhythmia while in the elevator, headed to his chest x-ray confirmation.
"He was revived and did fine, but it was kind of a scare to the whole hospital," recalled Racadio, who joined the staff shortly thereafter. "They basically said, 'Well, these new PICC things, they're too dangerous."
Even with the availability of portable radiography, the interventionalists' suggestion that all PICCs be placed in their suites appeared to be a cost-effective option, compared to having the PICC nurses making bedside microadjustments based on repeated x-rays and repeated phone calls to radiology.
Chest x-rays also have a visualization disadvantage compared to fluoroscopy for catheter placement, Racadio noted.
"The place where you see the tip on chest x-ray is actually falsely proximal. The true tip is actually further down," he said. "There’s no better way to view the exact tip of a catheter location than real-time fluoroscopy, where you can actually watch the catheter moving with heartbeat."
The Cincinnati facility has an interdisciplinary PICC program, teaming interventional radiology with six specially trained nurses. In straightforward cases where a vein can be palpated, the nurse can place the catheter under radiologist's supervision. In about 30% of cases, the radiologist needs to use ultrasound to gain access to the basilic vein.
Bedside interaction regarding PICCs remains important, however. The Cincinnati team developed a special educational chat and picture book on the procedure so that patients and parents are relaxed upon their arrival in the interventional suite.
"Because of all this pre-procedure education, we’ve actually been able to do our PICCs at Children's only having to sedate 6% of patients," Racadio said. Racadio is proudly sharing his experience with conservative sedation at medical meetings, noting that such stats are "not the norm around the country and around the world."
By Tracie L. Thompson
AuntMinnie.com staff writer
July 9, 2004
Related Reading
PICCing sides: Interventional radiologists weigh IV access lines, February 24, 2003
Copyright © 2004 AuntMinnie.com