Cancer patients who respond to neoadjuvant therapy have a better prognosis than nonresponders, of course, but with the exception of FDG-PET, reductions in the size of tumors treated with chemotherapy or radiation have been difficult to gauge using imaging modalities that are capable of delineating the anatomy.
Thanks to recent improvements in automated volumetry software, however, CT has the potential to measure response in a variety of settings. Examples to date include a 2006 study showing limited success assessing tumor response to treatment of esophagogastric junction cancers with CT volumetry, and a study that accurately measured changes in lung cancer tumors following radiation therapy.
In a study presented at the 2009 European Congress of Radiology (ECR), MDCT with automated volumetry accurately measured size changes in the lymph nodes of patients undergoing treatment for advanced gastric cancers.
"The purpose of our study was to evaluate the feasibility and reproducibility of automated CT volumetry for the prediction of histopathologic response to neoadjuvant chemotherapy of malignant lymph nodes in advanced gastric cancer patients," said Dr. M. Yu from Seoul National University in Seoul, South Korea.
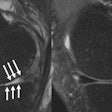
Forty-one patients were prospectively enrolled in the study, all with a diagnosis of advanced gastric cancer (AGC) with local lymph node metastasis but no distant metastases. The cohort underwent contrast-enhanced MDCT imaging both before and after chemotherapy. A radiologist prospectively determined the largest lymph node in each patient before treatment, which was deemed the index lymph node (iLN). All iLN were 8 mm or larger.
"Within one month after chemotherapy, right-side [access] gastrectomy was performed and the index lymph node was carefully dissected," Wu said. "Then, two GI pathologists determined the pathologic response of the index lymph node on a five-point scale from grade 0, normal lesion, to grade 4, tumorous lesion."
The 82 MDCT datasets (including before and after scans for each patient) were transferred to a workstation and processed with automated volumetry software (syngo CT Oncology, Siemens Healthcare, Erlangen, Germany).
"Two GI radiologists automatically measured the longest diameter and volume of the index lymph node," she said. The initial segmentation quality was graded on a scale from poor to excellent, and the number of verifications was recorded. Percentage diameter, area, and volume reduction rates were then calculated and correlated with pathologic regression grades.
The two radiologists also measured the diameter of the longest lymph node manually and then calculated the volume using a formula. In most cases, initial segmentation quality was high and no additional editing was performed. In other cases, manual measurements of the index lymph node according to Response Evaluation Criteria in Solid Tumors (RECIST) criteria overestimated the size, so additional manual editing and verification was needed, Wu said.
The percentage reduction in iLN size was correlated using Bland-Altman and Pearson correlations, compared between manual and automated methods.
In 82 iLNs, the results showed a mean score for initial automated segmentation quality of 3.4 ± 0.67. Fifty-nine percent of cases with initial segmentation scores of 2 or 3 required no additional verifications, while the remaining 41% (n = 34) cases required a mean of 1.51 and 1.87 verifications for the two radiologists, respectively. For these cases, the initial segmentation scores were 1.85 ± 1.13 and 1.78 ± 1.13, respectively.
Among the four measurement methods, percentage reduction rates for automatically calculated area and volume showed significant correlation with pathologic regression grades. The correlation coefficient was highest in the percentage volume reduction rate (r = 0.434, p = 0.008).
The automated measurements "showed a higher correlation coefficient than manual measurements for both RECIST and volume," Wu said. "Bland-Altman tests also showed better agreement in automated measurements than manual measurements for both RECIST and volume."
Automated CT volumetry is technically feasible for the assessment of lymph nodes, she concluded. "Automated CT volumetry of index lymph nodes is the most accurate tool in the prediction of histopathologic response following neoadjuvant chemotherapy in AGC," she said.
By Eric Barnes
AuntMinnie.com staff writer
March 27, 2009
Related Reading
NELSON lung cancer trial yields positive early results, March 9, 2009
New RECIST guidelines published, January 21, 2009
Perfusion CT predicts treatment response for pancreatic cancer, January 2, 2009
Measuring lung nodule growth beyond variability, November 5, 2007
Radiologists no match for nodule measurement software, August 31, 2007
Copyright © 2009 AuntMinnie.com