Where there's smoke, there's fire. Where there's long-term exposure to cigarette smoke in the lungs, you'll also find calcium -- and a heightened risk of lung cancer.
Just as coronary artery calcium is a reliable predictor of adverse events in the heart, researchers say that measuring calcifications in lung regions that receive the highest doses of cigarette smoke over time can sensitively predict the presence of all kinds of lung cancers.
Ricardo Avila and colleagues from Clifton Park, NY-based software developer Kitware, like other research teams, are looking for ways to predict the presence of lung cancer that improve upon the current, tedious practice of following solitary pulmonary nodules with CT over time until they look dangerous enough to biopsy.
In a special "hot topic" presentation at the 2008 RSNA meeting, Avila said that the presence of calcification at airway bifurcations in CT images can potentially predict the presence of lung cancer in smokers and former smokers who are screened with CT. His company is developing software to exploit the predictive power of such calcifications.
"It's pretty well established that lung cancer incidence is preceded by repeated exposure to cigarette smoke, and that there are many preneoplastic changes in the lungs in the decades prior to the incidence of lung cancer," Avila said. "Our approach is to measure preneoplastic changes in the regions that receive some of the greatest exposure to the cigarette smoke inhalation."
That region would be the airway bifurcation, according to environmental health literature that is based on histology as well as computational fluid dynamics. "Up to 100 times greater doses occur at the airway bifurcation and respiratory bronchials," Avila said.
Meanwhile, other studies on environmental toxin exposure show that lung damage occurs due to particulate matter deposition, which is a product of airflow dynamics as well as the deposition characteristics of the particulate matter, he said.
"Bifurcations in peripheral tissues are likely to exhibit some of the earliest preneoplastic changes in response to particulate matter exposure," Avila said. "It's also important to know that airways are composed in part of cartilage rings, and that these rings, particularly hyaline cartilage, have a propensity to calcify when stressed both biomechanically and from toxic exposure."
The researchers developed a lung cancer risk index (LCRI) based on two features, Avila explained.
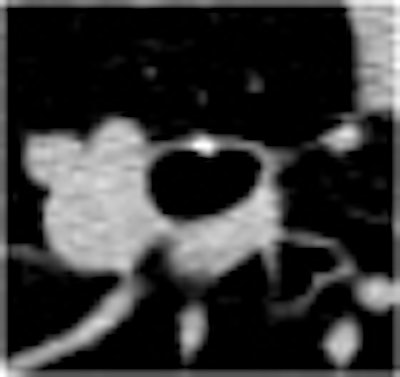
"One is something I'm calling a bifurcation damage index [BDI] which is a log scale. We measure [the bifurcation region] with high-resolution CT using an edge-enhancing kernel, and we take the average of five airway bifurcations in the lungs: two on the left, two on the right, and one on the ... first bifurcation of the trachea," he said.
In an effort to isolate the proportion of calcification that is due to particulate matter deposition, the algorithm subtracts the calcium score of a region above the bifurcation from the maximum pixel densities in the bifurcation regions of interest.
"Then we take the log of that [result] to come up with bifurcation damage index," Avila said.
The other feature in the LCRI measure consists of two common lung function measures: forced vital capacity (FVC), which measures the maximum amount of air an individual can expel after maximum inhalation, and forced expiratory volume in one second (FEV1), which is the amount of air the patient can expel in one second.
"There's a strong association between very low FEV1/FVC and cancer risk ... some studies have reported up to four times increased odds of developing lung cancer," Avila said.
And lung function measures combined with the bifurcation damage index are far more predictive of lung cancer than either measure alone, which is why the LCRI score is based on both modalities.
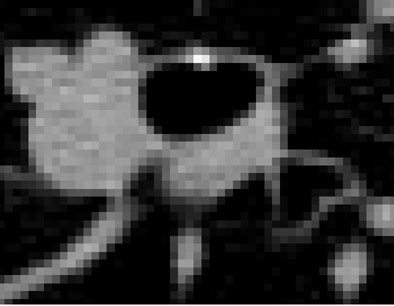 |
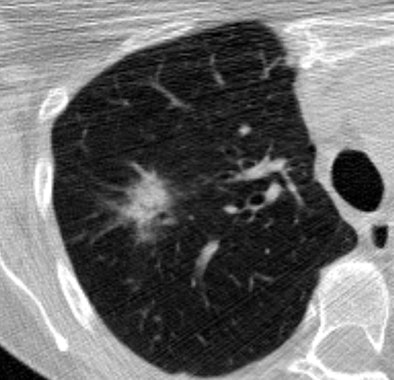
| CT image above shows extensive calcification along the carinal ridge of an airway bifurcation. The image is displayed without interpolation so that individual pixels are easily discerned. The peak voxel density along the carinal ridge shown in the slice is 614 HU. The DICOM header reveals that the CT data were acquired at 80mA, 120 kVp, 1.25-mm slice thickness, and with the bone kernel on a LightSpeed Ultra scanner (GE Healthcare, Chalfont St. Giles, U.K.). The bone kernel is not edge-enhancing, so the observed density cannot be due to the kernel; the densities were likely reduced due to partial volume artifact (the 614 HU voxel is adjacent to air). Image below from the same dataset case shows a part-solid lesion in the upper lobe of the right lung. All images courtesy of the Public Lung Database to Assess Drug Response. |
 |
The study examined 15 lung cancer patients and 93 individuals with a negative result from a cohort of 108 patients screened at an I-ELCAP (International Early Lung Cancer Action Program) site at the University of Navarra in Navarra, Spain. The cancers included a wide range of histologies, including small cell lung cancers, and multiple stages but mostly stage I, Avila said.
The patients with a lung cancer diagnosis were matched by age and pack years to the controls, and all but two patients were imaged using a B60f (edge-enhancing) reconstruction kernel on a Siemens Healthcare (Malvern, PA) scanner, Avila said.
LCRI measurements of all 108 cases found a lung cancer detection sensitivity and specificity of 67% and 72%, respectively. The same measures rose to 100% and 74%, respectively, when only the 79 cases scanned at 1-mm collimation were included in the analysis.
Lung cancer risk rose with the amount and length smoked. The mean LCRI values for 10-29, 30-49, 50-69, and ≥ 70 pack-year controls were 2.34, 2.46, 2.60, and 2.59, respectively.
Overall, 59% of the control cases had an LCRI value below the lowest cancer-positive LCRI value. This increased to 55/74 (74%) when applied to the subset of 79 cases where FEV1/FVC was greater than 50% and CT section thickness was 1.0 mm rather than 1.25 mm.
The odds ratio was 1.84 for every 0.1 increase in the lung cancer risk index (p = 0.0067). This ratio increased to 2.88 (p = 0.0467) when only cases scanned at 1-mm collimation were considered.
"Five of the cancers that had low [LCRI] values all had 1.25-mm slices [which suggests] that we're dealing with partial-volume artifact" in the cases imaged with 1.25-mm slices, Avila said.
"We have a new quantitative imaging biomarker based on airway bifurcation x-ray density," Avila concluded. A variant of this measure, the bifurcation damage index, is a manual measurement at this point but will eventually be automated, he said.
"The lung cancer risk index has high discriminatory power ... and we have evidence of being able to provide information about both lung cancer and [chronic obstructive pulmonary disease]," he said. "We believe that individual lung cancer risk is potentially quantifiable."
The results need to be confirmed in a larger number of cancer cases from a different location, he said. More emphasis should be placed on obtaining thinner slices with edge-enhancing filters, and the data suggest that better reconstruction kernels could improve lung cancer detection with CT.
Finally, "the field of aerosol science provides numerous insights, and we should be paying more attention to that research," Avila said.
By Eric Barnes
AuntMinnie.com staff writer
December 16, 2008
Related Reading
PET SUV measurements vary between facilities, December 10, 2008
Dual-energy CT helps distinguish PE from other perfusion defects, December 2, 2008
Measuring lung nodule growth beyond variability, November 5, 2007
Lung CAD holds up well in low-dose MDCT studies, November 25, 2008
CT databases aimed at lung imaging research, August 8, 2008
Copyright © 2008 AuntMinnie.com