The visualization of pericardial fluid associated with myocardial infarction, long the exclusive province of cardiac MRI, can be performed using CT, say researchers from Germany.
Differentiating acute from chronic myocardial infarction (MI), and detecting at-risk myocardium that may benefit from reperfusion therapy after acute MI, require important clinical decision-making. Several studies have proved the value of detecting myocardial edema on T2-weighted cardiac magnetic resonance (CMR) for differentiating acute from chronic MI. But while late-enhancement CT can now be used for depicting myocardial infarction (delayed contrast enhancement on late-phase CT directly shows necrotic myocardium), there is little data with regard to CT of myocardial edema.
"From early studies on CT imaging of MI, it is known that acute MI may present as areas of reduced CT values on unenhanced CT," wrote Dr. Andreas Mahnken and colleagues from the University of Aachen in Germany. "Theoretically, increased water content should result in a decrease of the CT value when compared with healthy myocardium" (JACC Cardiovascular Imaging, October 2009, Vol. 2:10, pp. 1167-1174).
The authors hypothesized that these areas of reduced attenuation values might correspond to myocardial edema rather than to MI. Their study, performed in seven pigs, sought to determine whether cardiac CT enables the assessment of myocardial edema in patients with acute MI.
 |
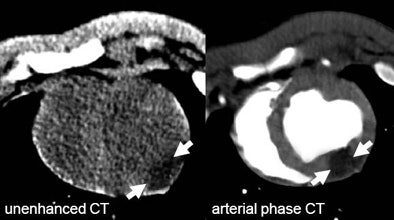 |
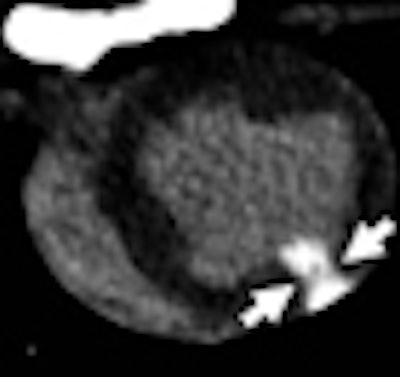
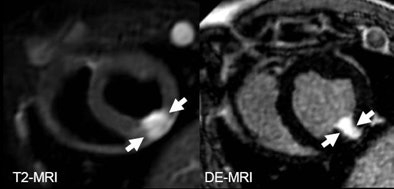
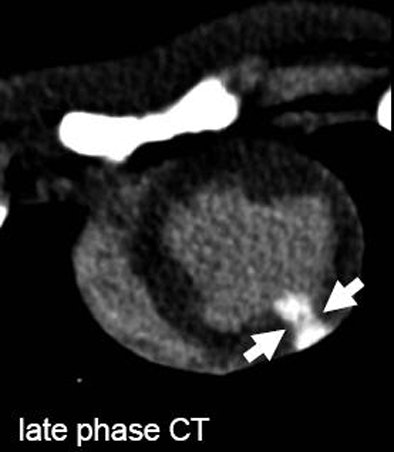
| The arrows on unenhanced CT show a hypodense area corresponding to edema as it can be seen on T2-weighetd MRI. The arrows on late-phase CT and MR correspond to infarction. The area of edema is larger than the area of infarction as expected based on previous MRI studies for the imaging of myocardial edema. All images courtesy of Dr. Andreas Mahnken. |
 |
After MI was induced in the animals using a closed-chest system, they underwent arterial and late-phase dual-source CT (DSCT).
CT data were acquired on a 64-slice DSCT scanner (Somatom Definition, release VA11, Siemens Healthcare, Erlangen, Germany), with all three scan phases performed craniocaudally during end-expiratory breath-hold. Standard settings included 120 kV for both tubes and 2 x 64 x 0.6-mm collimation for both detectors, rotation time of 330 msec, and heart rate-adapted pitch that ranged from 0.25 to 0.48. CT doses (in CTDIvol) ranged from 31.40 to 54.61 mGy.
Unenhanced CT was followed by arterial-phase imaging after administration of 120 mL of iopromide (Ultravist 300, Bayer Healthcare Pharmaceuticals, Wayne, NJ) and a delayed-phase scan 10 minutes later.
The investigators reconstructed double-oblique, 6-mm, short-axis images at 70% of the RR interval, with temporal resolution of 83 msec.
T2-weighted and delayed contrast CMR was performed on a clinical 1.5-tesla whole-body MR scanner (Gyroscan Intera, Philips Healthcare, Andover, MA) equipped with a dedicated five-element cardiac synergy coil.
After the two studies were complete, the animals were sacrificed and their hearts were excised and stained with 2,3,5-triphenyltetrazolin chloride (TTC). Mahnken and colleagues measured the size of MI, contrast-to-noise ratio, and percent signal difference among the different imaging techniques using concordance-correlation coefficients, Bland-Altman plots, and analysis of variance for repeated measures.
Twenty-nine CT, MR, and TTC sections presented with signs of ischemic injury, and in all slices, the infarction was transmural, Mahnken and colleagues noted.
According to the results, mean MI sizes on unenhanced, arterial, and late-phase DSCT were 27.2 ± 8.5%, 20.1 ± 6.9%, and 23.1 ± 8.2%, respectively. The corresponding values on T2-weighted and delayed enhanced CMR were 28.5 ± 7.8% and 22.2 ± 7.7%. Size of MI on TTC staining was 22.6 ± 7.8%.
The best agreement was found in the comparison between late-phase CT (pc = 0.9356) and delayed enhanced CMR (pc = 0.9248) with TTC staining. The group also found substantial agreement between unenhanced DSCT and the T2-weighted CMR images (pc = 0.8629).
Unenhanced DSCT offered the lowest percent signal difference (46.0 ± 18.3) and the lowest contrast-to-noise ratio (4.7 ± 2.0) between infarcted and healthy myocardium, they reported.
The study shows that "unenhanced DSCT provides different information about acute ischemic injury when compared with arterial and late-phase CT," Mahnken et al wrote. "Simple theoretical consideration led to the hypothesis that hypodense areas within the [left ventricular (LV)] myocardium correspond to edema, because increased tissue water content should result in a decrease of the CT values when compared with healthy myocardium."
The hypothesis is supported by the strong correlation with areas of edema on T2-weighted CMR, which are not to be confused with strongly hypodense areas on unenhanced CT. These are thought to correspond to fatty infiltrations that occur in chronic MI.
"In contrast, myocardial edema occurs in acute MI and presents with CT values > 0 HU," they wrote. But like CMR, CT overestimates infarction size.
One problem with the assessment of myocardial edema with DSCT is that the differences in CT values are low, "resulting in the need to apply high tube-current time products to keep the image noise in acceptable ranges" and to provide an acceptable contrast-to-noise ratio, the authors noted. As a result, the study requires the same radiation exposure as coronary CT angiography, although lower-dose prospective gating can be used in this application as well, they stated.
In addition there are no reference values for differentiating areas of edema from healthy myocardium; for this study, a difference of 12 HU was chosen arbitrarily. In addition, because all MI was transmural, subendocardial MI was not assessed.
"Unenhanced DSCT permits the detection of myocardial edema in acute MI," the researchers concluded. "This technique can be combined with arterial and late-phase CT, potentially enhancing the diagnostic utility of cardiac CT as an imaging modality for a comprehensive workup of patients with suspected myocardial ischemia."
Further studies are needed to confirm the findings; the group hopes to apply the technique in human studies beginning in 2010.
By Eric Barnes
AuntMinnie.com staff writer
December 17, 2009
Related Reading
Echocardiography test beats SPECT for predicting problems after MI, December 7, 2009
Coronary CTA edges CMR in a tight race, December 1, 2009
CMS takes comments on MRA policy, October 9, 2009
Cardiac MR techniques improve myocardial assessment, June 15, 2009
Contrast-enhanced CT finds myocardial infarction, June 10, 2004
Copyright © 2009 AuntMinnie.com



















