The research group used multiple 3 x 18-mm plastic tubing and stents in a 320-detector-row scanner (Aquilion One, Toshiba America Medical Systems, Tustin, CA) to perform the experiment, according to lead investigator Dr. Karl Coyner, Ph.D.
"We simulated stenoses inside of stents by using plastic plugs with predefined inner parameters, so we know exactly what the stenosis is," Coyner told AuntMinnie.com. "Then we were able to inject contrast through the catheter tubing, through the stent and out the other end. So you can imagine when you try to put contrast through a smaller hole, it takes longer to get through, so Hounsfield units or darkness over time changes. What we found was that this change was predictable, and that we could actually measure it with CT."
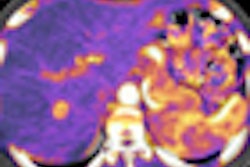
Coyner, along with Dr. Frank Rybicki and colleagues, oriented the stents and catheter tubing along the z-axis of the scanner and sequentially flushed them with a two-phase injection consisting of saline followed by diluted mixtures of iodine contrast and saline injected at 0.5 cc/sec; a one-second continuous dynamic volume acquisition during the injection enabled imaging of the advancing flow of contrast, the authors noted.
Repeated acquisitions were performed with simulated area stenoses (< 50%, 70%-85%) created by either circumferentially deforming the stents or by placing segments of tubing within the lumen. Hounsfield units (HU) were measured on cross-sectional images at regions of interest perpendicular to the lumen axis both proximal and distal to each stent.
Ex vivo dynamic flow imaging through the stents showed no flow compromise for lesions with < 50% stenosis, but diminished flow for the 70%-85% lesions, they reported. Thus, flow differences were quantified by the computed rise times and increased delay times distal to the stent.
"We don't know the ground truth," Rybicki said of the study's limitations. "We can only show that as the hole gets smaller, the flow changes more and more," but it hadn't been done before, he said. Thus, the experiment provides a model to measure flow across lesions with MDCT, he said.