Pulmonic Stenosis:
View cases of pulmonic stenosis
Clinical:
Pulmonic stenosis may be valvular, subvalvular, or supravalvular.
Supravalvular is the most common (60%) and the narrowing can occur anywhere from the pulmonary trunk to the segmental arteries [1]. Supravalvular pulmonic stenosis can be seen in association with Williams syndrome (abnormal facial appearance, mental retardation, and supravalvular aortic stenosis), Ehlers-Danlos syndrome, or post-Rubella syndrome [1]. Supravalvular stenoses can be classified as one of four types: Type I involves a single stenosis of the main, right, or left pulmonary arteries without peripheral branch involvement. Type II involves stenosis at the bifurcation of the pulmonary trunk extending into the origins of the right and left pulmonary arteries, without branch involvement. Type III involves multiple stenosis of the peripheral pulmonary artery branhces without central involvement. Type IV involves a combination of central and peripheral pulmonary artery stenoses [1].
Pulmonary valvular stenosis is a congenital disorder in 95% of
cases [2]. In
most patients, pulmonic valvular stenosis (PVS) is an
isolated
anomaly that
does not present until adulthood. Pulmonic valvular stenosis (PVS)
can
also be associated
with congenital heart disease- particularly tetrology of Fallot,
rheumatic heart disease
(rare), infective endocarditis (tricuspid valve is concomitantly
infected in 50% of cases) [4], or carcinoid syndrome (variable
pulmonic valve involvement is
found in up to 50-60% of
patients and is secondary to vasoactive amines producing a
superficial
endocarditis- classically both the tricuspid and pulmonary valve
leaflets are involved [4]).
Patients with Noonan's syndrome (mental retardation, web neck, and
short stature) also
have an increased incidence of pulmonic valvular stenosis- found
in up
to 30% of cases.
Patients with mild to moderate PVS generally have few symptoms.
Symptoms occur at a variable valve gradient, but most patients
with a peak gradient of less than 25 mm Hg are usually
asymptomatic [4]. With
more severe stenosis
there is right ventricular hypertrophy and later enlargement and
failure. Patients with severe stenosis can present with dyspnea,
fatigue, chest pain, and decreased exercise tolerance [4].
A normal pulmonary valve area measures approximately 2 cm [3].
The most common type of pulmonic stenosis (40-60% of cases) is a
dome-shaped pulmonary valve [4]. It is characterized by a mobile
valve with two to four raphes and incomplete separation of the
valve cusps which creates a funnel shape with a small circular
orifice [4]. Dysplastic pulmonary valve is the second most common
type (20-30% of cases) [4]. It is associated with thickened,
immobile cusps and, in some cases, a hypoplastic
ventriculo-arterial junction [4]. Cauliflower-like myxomatous
thickening is limited to the free margin of the leaflets (the
proximal part of the leaflet is intact) [4]. The commissures are
not fused [4]. A bicuspid valve is rare (0.1% of hearts) [4].
X-ray:
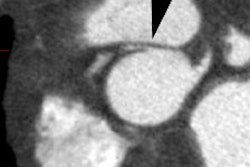
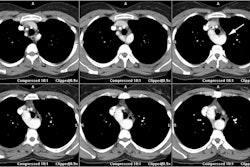
Post-stenotic dilatation of the main pulmonary artery is seen only in pulmonic valve stenosis. The degree of dilatation appears to be independent of the severity of the right ventricular outflow tract obstruction. A preferential 'jet-streaming' of blood across the stenotic pulmonic valve can result in asymmetric blood flow which is most commonly increased to the left lung (a classic finding in PVS). There will be associated asymmetric enlargement of the left pulmonary artery. Valve calcification is rare in PVS. MRI will demonstrate the turbulent jet as focal signal dropout in the left and main pulmonary artery segments, with normal laminar flow in the right pulmonary artery.
Patients with supra-valvular stenosis also typically have normal pulmonary blood flow on CXR. Patients with subvalvular, or infundibular, stenosis, however, typically have tetrology of Falot and therefore demonstrate decreased pulmonary blood flow.
REFERENCES:
(1) AJR 2000; Gamboa P, et al. Congenital multiple peripheral pulmonary artery stenosis (pulmonary branch stenosis or supravalvular pulmonary stenosis). 175: 856-857
(2) Radiographics 2009; Chen JJ, et al. CT angiography of the
cardiac valves: normal, diseased, and postoperative appearances.
29:
1393-1412
(3) J Cardiovasc Comput Tomogr 2012; Buttan Ak, et al. Evaluation
of
valvular heart disease by cardiac computed tomography assessment.
6:
381-392
(4) Radiographics 2014; Saromi F, et al. CT and MR imaging of the pulmonary valve. 34: 51-71