Shoulder ultrasound findings frequently have a significant effect on management and clinician decision-making in patients being treated for shoulder pain, according to research from the Mallinckrodt Institute of Radiology (MIR) in St. Louis.
After retrospectively evaluating the impact of more than 900 shoulder ultrasound exams on patient management, the Mallinckrodt researchers found that nearly two-thirds of patients received a change in their treatment plan based on the ultrasound findings. What's more, shoulder ultrasound had a statistically significant effect on the invasiveness of the patient treatment.
Dr. Michael Friedman shared the MIR research during a session at RSNA 2016 in Chicago.
A common complaint
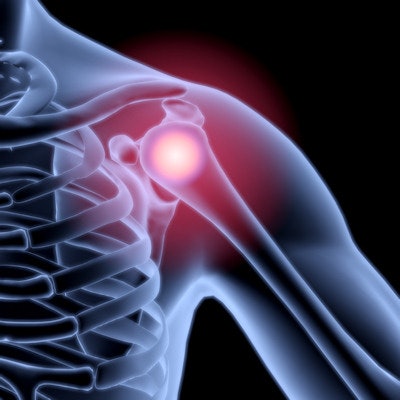
Shoulder pain is the third most common presenting musculoskeletal complaint after knee and low-back pain, affecting 16% to 26% of the population. It's a difficult clinical assessment, however, due to the overlap of many common shoulder pathologies, Friedman said.
Rotator cuff pathology is one of the most common causes of shoulder pain, for which MRI has been the gold standard. There's been a tremendous increase in the use of musculoskeletal ultrasound over the past five to 10 years, however. This growth is supported by research, such as a study that found 84% sensitivity and 89% specificity for partial-thickness tears and 96% sensitivity and 93% specificity for full-thickness tears, he said. MSK ultrasound also has been shown to have good correlation with MRI for rotator cuff muscular atrophy.
The Society of Radiologists in Ultrasound has published a consensus statement of recommended imaging algorithms for referring physicians on how to assess shoulder pain. Questions remain, however, about the actual diagnostic impact of musculoskeletal ultrasound on current orthopedic clinical evaluation of these patients.
As a result, the Mallinckrodt researchers set out to explore the effect of musculoskeletal ultrasound of the shoulder on clinical decision-making at their institution. A search of their RIS database found 1,037 consecutive shoulder ultrasound studies over a 12-month period, ordered by 15 orthopedic faculty members and interpreted by 10 radiologists. After 102 exams were excluded due to missing pre- and postultrasound clinical notes or because they were ordered for contralateral comparisons, the researchers were left with 935 patient exams for their study.
Three musculoskeletal radiologists then analyzed the electronic medical record and clinic notes and recorded the pre- and postultrasound treatment plans. Patients were classified into treatment plan categories, including conservative management/physical therapy (PT), therapeutic injection, or surgical intervention. Many patients were frequently prescribed conservative management/physical therapy and therapeutic injection together, which was also analyzed as a distinct management plan.
Conservative management/PT was considered to be noninvasive management, while therapeutic injection and surgical intervention were deemed to be invasive management.
Treatment changes
After receiving an ultrasound scan, 63.2% of patients had their treatment plans changed.
| Patient management plans before and after MSK ultrasound | ||
| Preultrasound treatment plan | No. of patients | Overall change in management plan following MSK ultrasound |
| Conservative management/PT | 744/935 (79.6%) | 490/744 (65.9%) |
| Invasive management (injection or scheduled for surgery) | 191/935 (20.4%) | 101/191 (52.9%) |
Of the 744 patients with an initial conservative management/PT treatment plan, 423 (56.9%) were shifted to a more invasive treatment plan based on the shoulder ultrasound exam. In patients set to receive an invasive management plan, 46 (24.1%) were changed to a noninvasive treatment plan.
The impact of shoulder ultrasound on the invasiveness of patient management was statistically significant (p < 0.001), Friedman said.
The researchers acknowledged the limitations of their study, including its reliance on the quality of physician documentation. The team did not make any assumptions about treatment intent and placed patients in treatment categories solely based on the impression in the clinical notes, Friedman said.
"This could easily be fixed by doing a prospective trial and by pulling in our orthopedic colleagues and letting them participate," he said.



















