Pulmonary Venoocclusive Disease:
Clinical:
Pulmonary venoocclusive disease (PVOD) is a rare disorder that results in pulmonary venous hypertension [11]. Pulmonary venoocclusive disease is a post-capillary cause of PAH [7].Some authors consider PVOD and pulmonary capillary hemagiomatosis to be different stages of the same disease (pathologic features of PCH are found in PVOD patients and findings of PVOD are found in 80% of PCH patients) [12]. Both disorders share the mutation of the EIF2AK4 gene (eukaryotic translation initiation factor 2 alpha kinase 4) located on chromosome 15, which could be responsible for the inherited PVOD and PCH with a recessive mode of transmission [12]. The gene codes for serine-threonine kinase, which induces changes in gene experssion in situations of amino acid deprivation, leading to a preferential synthesis of stress proteins [12]. This mutation is found in about 25% of sporadic cases of PVOD and PCH [7].
In sporadic cases, there may be an autoimmune component as the condition is associated with viral infection, environmental toxins, chemotherapy (carmustine,bleomycin, mitomycin), autoimmune disease (SLE, scleroderma, RA), oral contraceptives, high estrogen levels during pregnancy, bone marrow/hematologic stem cell transplant, radiation injury, and genetic predisposition.
Histologically there are webs, organized and recanalized thombosis, and intimal fibrosis within the pulmonary veins and venules [4,9,10]. Lumenal narrowing and subsequent obliteration/thrombosis lead to pulmonary hypertension [12]. Capillaries are typically dilated and engorged in patients with PVOD, but evolution of the disease could lead to a secondary angioproliferative process and capillary lesions which are characteristic of PCH [12].
Most cases occur prior to middle age (one-third of cases occur in children [4]), and the condition has also been reported in infants. Approximately 30-50% of patients are under the age of 20 years and in this group of patients there is no sex predilection [8]. Among adult patients, men are affected twice a s frequently as women [8].
Patients present with the insidious onset of orthopnea, episodes of acute pulmonary edema [9], fatigue, progressive dyspnea, and syncope. Unlike pulmonary capillary hemangiomatosis, PVOD is not associated with hemoptysis or hemorrhagic pleural effusions [8].
Clinically, the triad of severe pulmonary artery hypertension, pulmonary edema, and normal or low pulmonary capillary wedge pressures have been thought to be diagnostic of the disorder [8]. Left atrial and left ventricular pressures are also normal [4,9]. Lung biopsy is contraindicated and can be life threatening due to a high risk of hemorrhage [12]. Non-invasive clues to the diagnosis include low diffusing capacity for carbon monoxide, resting hypoxemia, severe oxygen desaturation on exercise, two or more characteristic features at CT (centrilobular ground glass opacitities, mediastinal lymph node enlargement, and/or smooth thickening of the interlobular septa), and occult hemorrhage at BAL [12].
The disorder is typically fatal within 2 years of diagnosis. Pediatric patients tend to experience a more rapid, relentless progression of disease [8]. No treatment has been effective, and bilateral lung transplant (or heart-lung transplant) is the only curative option (there has not be a report of recurrent disease following transplant)[8,12]. Supportive treatment until transplant consists mainly of O2 administration to avoid worsening of the pulmonary hypertension due to hypoxemia pulmonary vasoconstriction [7]. High doses of diuretics are recommended to prevent pulmonary edema [7]. Treatment with intravenous vasodilators used for pulmonary arterial hypertension (such as epoprostenol - a prostacyclin pathway activator, or calcium channel blockers) can be fatal [3,4,6]. Prostacyclin is a potent vasodilator [6]- if the pulmonary arterioles become dilated while the resistance of the pulmonary veins remains fixed, an increased in transcapillary hydrostatic pressure may result and produce florid pulmonary edema [6].
X-ray:
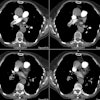
On CXR, patients demonstrate enlarged central pulmonary arteries characteristic of pulmonary arterial hypertension associated with the presence of Kerley lines, but no evidence of vascular redistribution to the upper lobes. On HRCT of patients with advanced disease, findings included evidence of PAH, interlobular septal thickening, ground glass centrilobular nodules [6], areas of ground-glass attenuation (central and gravity-dependent), a mosaic pattern of attenuation, small central pulmonary veins, and pleural effusions [4].V/Q imaging is generally not useful as a wide variety of findings can occur [8]. When abnormal, the most common pattern for PVOD (and pulmonary capillary hemangiomatosis) is patchy perfusion defects [13].
REFERENCES:
(2) Seminars in Roetgenology 1989; The pulmonary veins. 24 (2) Apr: 127-140 (No abstract available)
(3) Thorax 1999; Peacock AJ. Primary pulmonary hypertension. 54: 1107-1118 (Review. No abstract available)
(4) Radiographics 2000; Frazier AA, et al. From the archives of the AFIP. Pulmonary vasculature: Hypertension and infarction. 20: 491-524
(5) Radiographics 2002; Engelke C, et al. High-resolution CT and CT angiography of peripheral pulmonary disorders. 22: 739-764
(6) AJR 2004; Resten A, et al. Pulmonary hypertension: CT of the chest in pulmonary venoocclusive disease. 183: 65-70
(7) Radiographics 2006; Castaner E, et al. Congenital and acquired pulmonary artery anomalies in the adult: radiologic overview. 26: 349-371
(8) Radiographics 2007; Pulmonary veno-occlusive disease and pulmonary capillary hemangiomatosis. 27: 867-882
(9) Radiographics 2010; Grosse C, Grosse A. CT findings in
diseases associated with pulmonary hypertension: a current review.
30: 1753-1777
(10) Radiographics 2012; Pena E, et al. Pulmonary hypertension:
how the radiologist can help. 32: 9-32
(11) Radiographics 2013; Porres DV, et al. Learning from the
pulmonary veins. 33: 999-1022
(12) Radiology 2020; Delhaye C, et al. Pulmonary veno-occlusive
disease and pulmonary capillary hemangiomatosis. 295: 240-244
(13) Radiology 2021; Remy-Jardin M, et al. Imaging of pulmonary hypertension in adults: a position paper from the Fleischner society. 298: 531-549